Abstract
Purpose
The aim of this study was to determine whether sense of coherence (SOC) at baseline predicts health-related quality of life (HRQoL) at 12–28-month follow-up among patients with coronary heart disease when controlled for sociodemographic and medical variables.
Methods
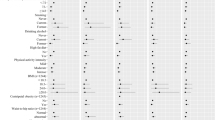
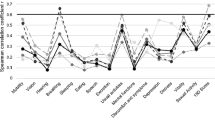
A total of 179 consecutive patients (58.28 ± 6.52 years, 16.8% women) scheduled for coronary angiography (CAG) were interviewed before CAG and 12–28 months after. SOC was measured with the 13-item Orientation to Life Questionnaire. HRQoL was measured using the Short Form Health Survey 36 (SF-36), from which the mental and physical component summaries (MCS, PCS) were calculated. The relationship between SOC and HRQoL was examined using regression analyses.
Results
SOC proved to be a significant predictor of the MCS-score (B = 0.29; 95% CI = 0.17–0.41) and PCS-score (B = 0.18; 95% CI = 0.06–0.31) when not adjusted for possible confounding sociodemographic and medical variables. After adjustment for sociodemographic and medical variables, SOC remained a predictor of the MCS-score (B = 0.26; 95% CI = 0.14–0.39). SOC also remained a predictor of the PCS-score when controlled for gender, age and family income; however, the association disappeared after adjustment for functional status (B = 0.07; 95% CI = −0.05 to 0.19).
Conclusions
SOC is a predictor of mental and physical HRQoL at 12–28-month follow-up, crude and also after adjustment. Patients undergoing CAG with low SOC thus deserve particular attention in regard to the maintenance and improvement of their HRQoL.

Similar content being viewed by others
Abbreviations
- HRQoL:
-
Health-related quality of life
- CHD:
-
Coronary heart disease
- SF-36:
-
Short form health survey questionnaire
- SOC:
-
Sense of coherence
- CAG:
-
Coronary angiography
- PCI:
-
Percutaneous coronary intervention
- CABG:
-
Coronary artery bypass grafting
- OLQ:
-
Orientation to life questionnaire
- PCS:
-
Physical component summary
- MCS:
-
Mental component summary
- NYHA:
-
New York Heart Association
- CCS:
-
Canadian cardiovascular society
- CI:
-
Confidence interval
References
Dantas, R. A. S., & Ciol, M. A. (2008). Quality of life after coronary artery bypass surgery. Western Journal of Nursing Research, 30(4), 477–489.
Spertus, J. A., Jones, P., McDonell, M., Fan, V., & Fihn, S. D. (2002). Health status predicts long-term outcome in outpatients with coronary disease. Circulation, 106(1), 43–49.
Weintraub, W. S., Spertus, J. A., Kolm, P., Maron, D. J., Zhang, Z., Jurkovitz, C., et al. (2008). Effect of PCI on quality of life in patients with stable coronary disease. The New England Journal of Medicine, 359(7), 677–687.
Loponen, P., Luther, M., Korpilahti, K., & Tarkka, M. (2009). HRQoL after coronary artery bypass grafting and percutaneous coronary intervention for stable angina. Scandinavian Cardiovascular Journal, 43(2), 94–99.
Ulvik, B., Nygard, O., Hanestad, B. R., Wentzel-Larsen, T., & Wahl, A. K. (2008). Associations between disease severity, coping and dimensions of health-related quality of life in patients admitted for elective coronary angiography: A cross sectional study. Health and Quality of Life Outcomes, 6(38), 1–12.
Dougherty, C. M., Dewhurst, T., Nichol, W. P., & Spertus, J. (1998). Comparison of three quality of life instruments in stable angina pectoris: Seattle Angina Questionnaire, Short Form Health Survey (SF-36), and Quality of Life Index-Cardiac Version III. Journal of Clinical Epidemiology, 51(7), 569–575.
Smith, H. J., Taylor, R., & Mitchell, A. (2000). A comparison of four quality of life instruments in cardiac patients: SF-36, QLI, QLMI, and SEIQoL. Heart, 84(4), 390–394.
Dempster, M., & Donelly, M. (2000). Measuring the health related quality of life of people with ischaemic heart disease. Heart, 83(6), 614–644.
Zuluaga, M. C., Guallar-Castillo, P., Lopez-Garcıa, E., Banegas, J. R., Conde-Herrera, M., Olcoz-Chiva, M., et al. (2010). Generic and disease-specific quality of life as a predictor of long-term mortality in heart failure. European Journal of Heart Failure, 12(12), 1372–1378.
Myint, P. K., Luben, R. N., Surtees, P. G., Wainwright, N. W. J., Welch, A. A., Bingham, S. A., et al. (2006). Relation between self-reported physical functional health and chronic disease mortality in men and women in the European Prospective Investigation into Cancer (EPIC-Norfolk): A prospective population study. Annals of Epidemiology, 16(6), 492–500.
Schenkeveld, L. S., Pedersen, S. S., van Nierop, J. W. I., Lenyen, M. J., de Jagere, P. P. T., Serruys, P. W., et al. (2010). Health-related quality of life and long-term mortality in patients treated with percutaneous coronary intervention. American Heart Journal, 159(3), 471–476.
Mossey, J. M., & Shapiro, E. (1982). Self-rated health: A predictor of mortality among the elderly. American Journal of Public Health, 72(8), 800–808.
Konstam, V., Salem, D., Pouleur, H., Kostis, J., Gorkin, L., Shumaker, S., et al. (1996). Baseline quality of life as a predictor of mortality and hospitalization in 5,025 patients with congestive heart failure. SOLVD investigations. Studies of left ventricular dysfunction investigators. American Journal of Cardiology, 78(8), 890–895.
Antonovsky, A. (1979). Health, stress and coping. San Francisco: Jossey-Bass.
Antonovsky, A. (1987). Unraveling the mystery of health. How people manage stress and stay well. San Francisco: Jossey-Bass.
Antonovsky, A. (1993). The structure and properties of the sense of coherence scale. Social Science and Medicine, 36(6), 725–733.
Karlsson, I., Berglin, E., & Larsson, P. A. (2000). Sense of coherence: Quality of life before and after coronary artery bypass surgery: A longitudinal study. Journal of Advanced Nursing, 31(6), 1383–1392.
Kattainen, E., Merilainen, P., & Sintonen, H. (2006). Sense of coherence and health-related quality of life among patients undergoing coronary artery bypass grafting or angioplasty. European Journal of Cardiovascular Nursing, 5(1), 21–30.
Motzer, S. U., & Stewart, B. J. (1996). Sense of coherence as a predictor of quality of life in persons with coronary heart disease surviving cardiac arrest. Research in Nursing and Health, 19(4), 287–298.
Guldvog, B. (1999). Can patient satisfaction improve health among patients with angina pectoris? International Journal for Quality in Health Care, 11(3), 233–240.
Klevsgard, R., Hallberg, I. R., Risberg, B., & Thomsen, M. B. (2000). The effects of successful intervention on quality of life in patients with varying degrees of lower-limb ischaemia. European Journal of Vascular and Endovascular Surgery, 19(3), 238–245.
Bruscia, K., Shultis, C., Dennery, K., & Dileo, Ch. (2009). Predictors of quality of life in hospitalized cardiac patients. Journal of Health Psychology, 13(8), 982–987.
Veenstra, M., Moum, T., & Roysamb, E. (2005). Relationship between health domains and sense of coherence: A two-year cross-lagged study in patients with chronic illness. Quality of Life Research, 14(6), 1455–1465.
Drory, Y., Kravetz, S., & Hirschberger, G. (2002). Long-term mental health of men after a first acute myocardial infarction. Archives of Physical Medicine and Rehabilitation, 83(3), 352–359.
Norekval, T. M., Fridlund, B., Moons, P., Nordrehaug, J. E., Saevareid, H. I., Wentzel-Larsen, T., et al. (2010). Sense of coherence: A determinant of quality of life over time in older female acute myocardial infarction survivors. Journal of Clinical Nursing, 19(5–6), 820–831.
Scarborough, P., Bhatnagar, P., Wickramasinghe, K., Smolina, K., Mitchell, C., & Rayner, M. (2010). Coronary heart disease statistics 2010 edition. London: British Heart Foundation.
Dantas, R. A. S., Motzer, S. A., & Ciol, M. A. (2002). The relationship between quality of life, sense of coherence and self-esteem in persons after coronary artery bypass graft surgery. International Journal of Nursing Studies, 39(7), 745–755.
Jarvinen, O., Saarinen, T., Julkunen, J., Huhtala, H., & Tarkka, M. R. (2003). Changes in health-related quality of life and functional capacity following coronary artery bypass graft surgery. European Journal of Cardio-Thoracic Surgery, 24(5), 750–756.
Pettersen, K. I., Reikvam, A., Rollag, A., & Stavem, K. (2008). Understanding sex differences in health-related quality of life following myocardial infarction. International Journal of Cardiology, 130(3), 449–456.
Bergman, E., Malm, D., & Karlsson, J. E. (2009). Longitudinal study of patients after myocardial infarction: Sense of coherence, quality of life, and symptoms. Heart and Lung, 38(2), 129–140.
Brink, E., Grankvist, G., Karlson, B. W., & Hallberg, L. R. (2005). Health-related quality of life in women and men one year after acute myocardial infarction. Quality of Life Research, 14(3), 749–757.
Lindsay, G. M., Hanlon, P., Smith, L. N., & Wheatley, D. J. (2000). Assessment of changes in general health status using the short form 36 questionnaire 1 year following coronary artery bypass grafting. European Journal of Cardio-Thoracic Surgery, 18(5), 557–564.
Lundberg, J., Karlsson, N., & Kristenson, M. (2009). Does two year stability for scale scores of psychosocial factors differ by socioeconomic position? Psychological Reports, 105(3), 1009–1022.
Simchen, E., Galai, N., Braun, D., Zitser-Gurevich, Y., Shabtai, E., & Naveh, R. N. (2001). Sociodemographic and clinical factors associated with low quality of life one year after coronary bypass operations. The Israeli Artery Bypass Study (ISCAB). Journal of Thoracic and Cardiovascular Surgery, 121(5), 909–919.
The Task Force on the Management of Stable Angina Pectoris of the European Society of Cardiology. (2006). Guidelines on the management of stable angina pectoris. Europen Heart Journal, 27(211), 1341–1381.
Skodova, Z., Nagyova, I., van Dijk, J. P., Sudzinova, A., Vargova, H., Rosenberger, J., et al. (2009). Socioeconomic inequalities in quality of life and psychological outcomes among cardiac patients. International Journal of Public Health, 54(4), 233–240.
Skodova, Z., Nagyova, I., Rosenberger, J., van Dijk, J. P., Middel, B., Vargova, H., et al. (2008). Vital exhaustion in coronary heart disease: The impact of socioeconomic status. European Journal of Cardiovascular Prevention & Rehabilitation, 15(5), 572–576.
Cohen, J. (1977). Statistical power analysis for the behavioural sciences. New York: Academic Press.
Eriksson, M., & Lindstrom, B. (2005). Validity of Antonovsky’ sense of coherence scale: A systematic review. Journal of Epidemiology and Community Health, 59(6), 460–466.
Read, S., Aunola, K., Feldt, T., Leinonen, R., & Ruoppila, I. (2005). The relationship between generalized resistance resources, sense of coherence, and health among finish people aged 65–69. European Psychologist, 10(3), 244–253.
Gana, K., & Garnier, S. (2001). Latent structure of the sense of coherence scale in a French sample. Personality and Individual Differences, 31(7), 1079–1090.
Ware, J. E., Kosinski, M., & Keller, S. D. (1994). SF-36 Physical and mental summary scales: A user’s manual. Boston: The Health Institute.
Failde, I., & Ramos, I. (2000). Validity and reliability of the SF-36 health survey questionnaire in patients with coronary artery disease. Journal of Clinical Epidemiology, 53(4), 359–365.
Criteria Committee of the New York Heart Association. (1994). Functional capacity and objective assessment. In M. Dolgin (Ed.), Nomenclature and criteria for diagnosis of diseases of the heart and great vessels (pp. 253–255). Boston: Little, Brown and Company.
Campeau, L. (1976). Garding of angina pectoris letter. Circulation, 54(3), 522–523.
Slovak Ministry of Social Affairs. (2009). Act No. 252/2009 Governmental Regulation of Minimum Wage. Retrieved July, 1, 2010, from http://www.employment.gov.sk/DIS/dis/index.php?SMC=1&id=170.
Nesbitt, B. J., & Heidrich, S. M. (2000). Sense of coherence and illness appraisal in older women’s quality of life. Research in Nursing and Health, 23(1), 25–34.
Eriksson, M., & Lindstrom, B. (2006). Antonovsky’s sense of coherence scale and the relation with health: A systematic review. Journal of Epidemiology and Community Health, 60(5), 376–381.
Ekman, I., Fagerberg, B., & Lundman, B. (2002). Health-related quality of life and sense of coherence among elderly patients with severe chronic heart failure in comparison with healthy controls. Heart and Lung, 31(2), 94–101.
Fok, S. E., Chair, S. Y., & Lopez, V. (2005). Sense of coherence, coping and quality of life following a critical illness. Journal of Advanced Nursing, 49(2), 173–181.
Eriksson, M., & Lindstrom, B. (2007). Antonovsky′s sense of coherence scale and its relation with quality of life: A systematic review. Journal of Epidemiology and Community Health, 61(11), 938–944.
Langeland, E., Riise, T., Hanestad, B. R., Nortvedt, M. W., Kristoffersen, K., & Wahl, A. K. (2006). The effect of salutogenic treatment principles on coping with mental health problems A randomised controlled tiral. Patient Education and Counseling, 62(2), 212–219.
Forsberg, K. A., Bjorkman, T., Sandman, P. O., & Sandlund, M. (2010). Influence of lifestyle intervention among persons with a psychiatric disability: A cluster randomized controlled trail on symptoms, quality of life and sense of coherence. Journal of Clinical Nursing, 19(11–12), 1519–1528.
Wiessbecker, I., Salmon, P., Studts, J. L., Floyd, A. L., Dedert, E. A., & Sephton, S. E. (2002). Mindfulness-based stress reduction and sense of coherence among women with fibromyalgia. Journal of Clinical Psychology in Medical Settings, 9(4), 297–307.
Lee, R. G., & Garvin, T. (2003). Moving from information transfer to information exchange in health and health care. Social Science and Medicine, 56(3), 449–464.
Acknowledgments
The authors would like to thank the patients with cardiological problems who participated in this study, and also Adriana Sudzinova MD, Helena Vargova MD, Antonia Halecka MD, Diana Matlakova, Eva Hackenberg and Zuzana Skodova PhD for their substantial help in the data collection. This work was supported by the Slovak Research and Development Agency under contract No. APVV-20-038305 (20%) and No. APVV-0220-10 (60%). Furthermore, this work was partially supported by the Agency of the Slovak Ministry of the Education, Science, Research and Sport of the Slovak Republic for the Structural Funds of the EU under project No. ITMS: 26220120058 (20%).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Silarova, B., Nagyova, I., Rosenberger, J. et al. Sense of coherence as an independent predictor of health-related quality of life among coronary heart disease patients. Qual Life Res 21, 1863–1871 (2012). https://doi.org/10.1007/s11136-011-0106-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-011-0106-2