Abstract
BACKGROUND
Failed referrals for specialty care are common and often represent medical errors. Technological structures and processes account for many failures. Scheduling appointments for subspecialty evaluation is a first step in outpatient referral and consultation.
OBJECTIVE
We determined whether moving from paper-based referrals to a Web-based system with automated tracking features was associated with greater scheduling of appointments among referred patients.
DESIGN
Staggered implementation of a quality-improvement project, with comparison of intervention and control groups.
PARTICIPANTS
Patients 21 or more years of age referred from any of 11 primary-care clinics to any of 25 specialty clinics.
INTERVENTIONS
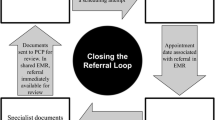
Faxed referrals were replaced by a Web-based application shared by generalists and specialists, with enhanced communications and automated notification to the specialty office.
MEASUREMENTS
We compared scheduling before and after implementation and time from referral to appointment. A logistic regression analysis adjusted for demographics.
MAIN RESULTS
Among 40,487 referrals, 54% led to scheduled specialty visits before intervention, compared to 83% with intervention. The median time to appointment was 168 days without intervention and 78 days with intervention. Scheduling increased more when duplicate referrals were not generated (54% for single orders, 24% for multiple orders). After adjustment, referrals with the intervention were more than twice as likely to have scheduled visits.
CONCLUSIONS
With a new Web-based referrals system, referrals were more than twice as likely to lead to a scheduled visit. This system improves access to specialty medical services.
Similar content being viewed by others
References
Linzer M, Myerburg RJ, Kutner JS, et al. Exploring the generalist-subspecialist interface in internal medicine. Am J Med. 2006;119(6):528–37.
Wilkin D, Smith A. Explaining variation in general practitioner referrals to hospital. Fam Pract. 1987;4(3):160–9.
Calman NS, Hyman RB, Licht W. Variability in consultation rates and practitioner level of diagnostic certainty. J Fam Pract. 1992;35(1):31–8.
Rosemann T, Wensing M, Rueter G, et al. Referrals from general practice to consultants in Germany: if the GP is the initiator, patients’ experiences are more positive. BMC Health Serv Res. 2006;6:5.
Cefalu CA. Adhering to inpatient geriatric consultation recommendations. J Fam Pract. 1996;42(3):259–63.
Ballard WP, Gold JP, Charlson ME. Compliance with the recommendations of medical consultants. J Gen Intern Med. 1986;1(4):220–4.
Allen CM, Becker PM, McVey LJ, et al. A randomized, controlled clinical trial of a geriatric consultation team. Compliance with recommendations. JAMA. 1986;255(19):2617–21.
Shah PN, Maly RC, Frank JC, et al. Managing geriatric syndromes: what geriatric assessment teams recommend, what primary care physicians implement, what patients adhere to. J Am Geriatr Soc. 1997;45(4):413–9.
Forrest CB, Glade GB, Baker AE, et al. Coordination of specialty referrals and physician satisfaction with referral care. Arch Pediatr Adolesc Med. 2000;154(5):499–506.
Committee on Quality of Health Care in America, Institute of Medicine. To Err is human: building a safer health system. In: Kohn LT, Corrigan JM, Donaldson M, eds. Washington, DC: National Academy of Sciences; 1999.
Wootton R, Harno K, Reponen J. Organizational aspects of e-referrals. J Telemed Telecare. 2003;9(Suppl 2):S76–9.
MindGent. MindGent Service Center. Available at: http://www.mindgent.com/. Accessed 03 June 2008.
Gandhi TK, Sittig DF, Franklin M, et al. Communication breakdown in the outpatient referral process. J Gen Intern Med. 2000;15(9):626–31.
Olivotto IA, Gomi A, Bancej C, et al. Influence of delay to diagnosis on prognostic indicators of screen-detected breast carcinoma. Cancer. 2002;94(8):2143–50.
Ordin D. QUERI II and VA performance improvement. “Forum” publication of VA Office of Research & Development 2006 (August); August 2006:3.
Moorman PW, Branger PJ, van der Kam WJ, et al. Electronic messaging between primary and secondary care: a four-year case report. J Am Med Inform Assoc. 2001;8(4):372–8.
Abbott KC, Mann S, DeWitt D, et al. Physician-to-physician consultation via electronic mail: the Walter Reed Army Medical Center Ask a Doc system. Mil Med. 2002;167(3):200–4.
Arenson R. Why bother with a computerized scheduling system? J Digit Imaging. 1988;1(1):24–7.
Mozumdar BC, Hornsby DN, Gogate AS, et al. Radiology scheduling: preferences of users of radiologic services and impact on referral base and extension. Acad Radiol. 2003;10(8):908–13.
Woods L. What works: scheduling. Picture perfect solution. The right technology and an ASP solution bring scheduling efficiency and added revenue to a community hospital's radiology department. Health Manag Technol. 2001;22(8):48–50.
Acknowledgements
Dr. Weiner was supported on this work by grant number 5K23AG020088 from the National Institute on Aging. Aspects of this work were presented at a meeting of the Midwest Region Society of General Internal Medicine, Chicago, IL, 30 September 2005. This study was supported by Wishard Health Services, Indianapolis, Indiana.
Conflicts of Interest
None of the authors have any conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Additional information
SUPPORT:
Dr. Weiner was supported by grant number 5K23AG020088 from the National Institute on Aging. This study was supported by Wishard Health Services, Indianapolis, Indiana.
Rights and permissions
About this article
Cite this article
Weiner, M., El Hoyek, G., Wang, L. et al. A Web-based Generalist–Specialist System to Improve Scheduling of Outpatient Specialty Consultations in an Academic Center. J GEN INTERN MED 24, 710–715 (2009). https://doi.org/10.1007/s11606-009-0971-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-009-0971-3