Abstract
Background
Medical scribes have been proposed as a solution to the problems of excessive documentation, work-life balance, and burnout facing general internists. However, their acceptability to patients and effects on provider experience have not been tested in a real-world model of effectiveness.
Objective
To measure the effect of medical scribes on patient satisfaction, provider satisfaction, and provider productivity.
Design
Quasi-experimental difference-in-differences longitudinal design.
Participants
Four attending physicians who worked with scribes, 9 control physicians who did not, and their patients in a large, hospital-affiliated academic general internal medicine practice.
Main Measures
Provider experience and patient experience using 5-point Likert scale surveys from the AMA Steps Forward Team Documentation Module, and visits and wRVUs per hour during 4 weeks before and 12 weeks after initiation of a practice model that included use of scribes and a shortened visit template.
Key Results
Participating providers worked a total of 664 clinic sessions and returned 547 (82%) surveys. Average provider experience scores did not differ between providers working with scribes and control providers working without (4.01 vs. 3.40 respectively; p time-by-group interaction = 0.26). Providers with scribes were more likely to agree that work for the encounter would be completed during the visit then controls (3.58 vs. 2.48 respectively; p interaction = 0.04). A total of 6202 visits occurred during the study period. Average patient experience scores did not differ between the experimental and control groups (4.73 vs. 4.75 respectively; p interaction = 0.90). Compared with the control providers, providers with scribes completed more visits per hour (2.29 vs. 1.91; p interaction < 0.001) and generated more wRVUs per hour (3.42 vs. 3.27; p interaction < 0.001).
Conclusions
In this test of a modified practice model, scribes supported greater patient throughput and improved provider perceptions of documentation burden with no decrement in high patient satisfaction.
Similar content being viewed by others
INTRODUCTION
Documentation, once a small part of the patient encounter, has grown to become a major driver of physician time. With increasing use of the medical record as an instrument for billing, and particularly with advent of the electronic health record (EHR), the medical note may seem as important as the actual patient care. This dynamic has a measurable negative effect on patient centeredness and physician work-life balance.1 For every hour that physicians provide direct clinical face time to patients, two additional hours are spent on EHR and desk work within the clinic day. Outside of office hours, physicians spend another 1 to 2 h of personal time daily performing additional computer and clerical work.2,3,4,5 A number of solutions to this largely uncompensated effort have been proposed, ranging from improving the usability of the EHR to medical scribes.6,7,8
A medical scribe is a non-clinical ancillary staff member who assists a licensed-independent provider. Duties include real-time transcribing of physician notes, organization of objective healthcare data, point-of-service collections, and patient tracking.9 Scribes have been employed in emergency departments since the late twentieth century7 and their use has grown steadily since. One recent editorial by the American College of Medical Scribe Specialties estimated “industry ranks to swell to 100,000 [scribes] by 2020.”8
A review of existing literature reflects this trend. Until recently, evidence on the benefits and tradeoffs of medical scribes has been limited to the emergency and ambulatory subspecialty practice settings.10,11,12 As recently as 2014, a meta-analysis concluded that “confidence in the reliability of the evidence is significantly constrained,” and called for “methodologically and sufficiently powered studies.” Since then, several studies examining the use of medical scribes in the primary care setting have been published. Collectively, these demonstrate benefit of medical scribes to providers, patients, and healthcare systems.13, 14 Despite promising results, these studies often lack generalizability and fail to provide crucial information about the effects of scribes on patient and provider satisfaction or how to accommodate the increased costs of employing scribes.
Here, we present the detailed results of a single-center, quasi-experimental study of the effect of medical scribes on patient satisfaction, provider satisfaction, and provider productivity. We focused on a real-world implementation model, in which provider workload was adjusted a priori to account for the increased costs incurred by scribes.
METHODS
Practice Setting
Healthcare Associates is a large, hospital-based academic general internal medicine practice. It is the primary teaching site for the Beth Israel Deaconess Internal Medicine Residency program. HCA serves a panel of over 40,000 patients and is staffed by 47 faculty and 120 residents comprising approximately 40 full-time equivalent (FTE). Standard clinic sessions are 4 h in length and include 20-min visits for follow-up and urgent care and 40-min appointments for new patients, annual physicals, and particularly complex follow-up visits. The practice is divided into four suites, each with its own team of physicians, medical assistants, nurses, and ancillary staff.
Study Participants
For this study, we evaluated scribes in one suite within HCA. Given funding limitations, we selected a convenience sample of four attending physicians to work with scribes and nine others in the same suite to serve as controls. Two scribes were provided by a large, nationally recognized scribe company. The first scribe was female with 1.5 years of experience and able to type 90 words per minute. The second scribe was male with 2.5 years of experience and able to type 110 wpm. Both had a bachelor’s degree. Providers in the intervention group shared both scribes to ensure 100% shift coverage. The same scribes were utilized throughout the study period. The scribe’s primary work duties were to provide real-time transcription of office visits and to organize and document clinical data reviewed by the clinician.
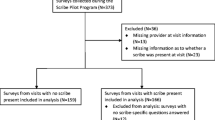
Intervention
We tested the effect of scribes using a difference-in-differences approach, in which we compared differences between intervention and control periods among physicians who used scribes with the corresponding differences among physicians who did not use scribes during the identical periods. We first evaluated physician and patient outcomes for 4 weeks at baseline, prior to any modification in the practice. We then implemented scribes in a transitional 3-week “honeymoon” period, in which scribes were provided to the four intervention physicians, but no change to standard visit lengths was made; this was intended to represent the expected period of adaptation for patients, physicians, and staff. Then, for the next 12 weeks, intervention physicians used scribes with their visit lengths shortened from 20 to 15 min and from 40 to 30 min, increasing the number of patient slots available in each 4-h session. Control physicians experienced no change to their visit lengths. No other significant changes occurred in the practice during this time period, and we made no change to staffing levels of medical assistants, nurses, telephone staff, or administrative assistants.
This study was reviewed by the BIDMC Committee on Clinical Investigation and did not meet the definition of Human Subjects Research.
Outcomes
We examined outcomes in three domains: provider experience, patient experience, and provider productivity.
We measured the provider experience using a survey recommended by the American Medical Association in its Steps Forward Team Documentation Module.15, 16 The survey was administered to each provider after each clinic session. Providers were asked to rate their agreement with the following statements using a 5-point Likert-like scale from (1) strongly disagree to (5) strongly agree: Q1: “I was able to provide the patient care needed without feeling rushed”; Q2: “I left the exam room feeling satisfied with the encounter”; Q3: “I left the exam room feeling that majority of work for the encounter would be completed by the end of the patient visit”; Q4: “I was able to give my patients my full attention”; and Q5: “Overall, I was able to stay on schedule.”
Because one of the four intervention providers (JH) played a role in study design (but not analysis), his satisfaction scores (but not other metrics) were excluded from all analyses.
We measured patient experience using a similar survey from the Steps Forward Team Documentation Module.15 The survey was administered to each patient after their visit at the time of checkout. Patients were asked to rate their agreement with the following statements using the same Likert-like scale as above: Q1: “I feel good about my medical visit”; Q2: “My doctor or provider gave me his/her full attention”; Q3: “I was able to say everything I wanted to say to my doctor or provider”; and Q4: “I understand the care recommendations that my doctor or provider gave me today.”
We assessed productivity using metrics of both patients seen per hour, to enable comparability irrespective of billing, and wRVUs per hour, which provide greater utility for financial purposes. For both control and intervention groups, we only included visits on regularly scheduled clinic days; ad hoc visits for single patients in off-hours, which were rare, were excluded. Because a few visits (primarily among control providers) had not been billed within 7 days at the conclusion of the study, we imputed wRVUs for those visits at the overall median value.
Statistical Analysis
We assessed the three sets of outcomes in similar fashion. For patient and provider satisfactions, we constructed generalized estimating equations assuming compound symmetry with outcomes of either the score on an individual question or the total summed score for all four or five questions. For productivity, outcomes constituted wRVU or visits per hour.
We clustered by provider and assumed Poisson’s distributions for individual scores and Gaussian distributions for total scores and productivity measurements. We present mean values from models that include indicator variables for study period, study group, and their multiplicative (i.e., time × treatment) interaction; we present p values for the latter terms. Productivity measures additionally adjusted for actual hours worked; analyses that did not adjust for hours worked or that modeled outcomes per day (rather than per hour) yielded very similar results that are not shown here.
We tested the assumption of parallel trends between groups during the baseline period using time in days (rather than study period). In all cases, we found no deviation from the assumption of parallel trends (p = 0.38 for average patient score, p = 0.46 for average provider score, p = 0.38 for wRVU per hour, and p = 0.89 for visits per hour). Because all models clustered by provider, results were also unchanged by adjustment for provider age, years in practice, and sex; as a result, results from primary models are shown.
Financial Analysis
To estimate the costs and benefits, we provide the hourly costs of scribes and the costs of travel and housing (required by the scribe company specifically for this study). We estimate a blended gain of $144.87 in professional revenue for each visit, based upon the observed distribution of evaluation and management codes in our practice. To estimate overall savings or losses, we multiplied the hourly cost of scribes by actual hours worked, added travel and housing costs, and compared these with the product of the incremental visit revenue multiplied by the difference-in-differences in patients seen.
RESULTS
Provider Experience
Table 1 shows provider characteristics according to the intervention group. Participating providers worked a total of 664 sessions and returned 547 (82%) surveys. Table 2 shows results for the overall scores and for each individual question. In general, scores improved more in the intervention group than among controls. These differences were statistically significant for feeling that work for the encounter would be completed during the visit. Of note, perception of being rushed and staying on schedule did not statistically deteriorate despite the shorter scheduled visit length among intervention participants.
Patient Experience
Among 6202 patient visits during the study period, we collected 2130 (34%) surveys. In general, patients reported a high level of satisfaction in both groups, with mean scores of approximately 4.7 out of 5 (Table 3). Despite the shorter visit duration in the intervention group, we observed no statistically significant differences between the two groups in any measure of patient satisfaction.
Provider Productivity
On average (standard deviation) in the baseline period, providers saw 2.0 (0.5) patients per hour, representing 3.4 (1.1) wRVU per hour. As seen in Table 4, we observed a marked increase in both patients seen and wRVUs accumulated per hour among providers working with scribes. In contrast, small declines in both metrics were observed among control providers, and the difference-in-differences was strongly statistically significant.
Financial Analyses
We paid a premium rate for scribes of $30/h per scribe plus $6000 negotiated flat rate to cover the costs of travel and housing for the study period. The study period lasted 806 h, for total costs of $30,000 (the a priori budget cap). Approximately 14% of scribe hours were spent on pre-visit planning and completion of documentation at the end of each day. Given that intervention practices increased by 0.45 visits per hour relative to controls, we estimate that this pilot period generated an additional $46,000 in collections, for a total estimated return on investment of $16,000.
DISCUSSION
We present a single-center quasi-experimental study of the effect of medical scribes on patient satisfaction, provider satisfaction, and provider productivity. Our study participants saw significantly more patients per hour then control providers without any decline in perceptions of being rushed or falling behind schedule. Furthermore, scribe use was associated with a significant improvement in physician perception of documentation burden. Patient experiences were generally outstanding and did not differ between the two groups, suggesting that the presence of a scribe did not negatively impact the primary care encounter. The estimated increase in productivity more than covered actual scribe costs for this study.
Scribes have been little-studied in general academic internal medicine until recently. What has been written supports our observations that medical scribes improve provider job satisfaction and efficacy without detracting from the patient experience.11, 12, 14, 17, 18 To date only one other study has examined the financial implications of a medical scribe program in an academic internal medicine practice, and it reported results similar to our own.13
Medical scribes are a means of increasing provider capacity by transferring documentation responsibility to a third party. Therefore, it is not surprising that providers using scribes reported improvement in perceptions related to documentation burden and completion of non-clinical tasks. While other domains did not improve to a statistically significant degree, it is worth noting that those domains did not decrease despite a significant increase in patient throughput. Because our study showed a net financial gain overall, this raises the question of whether slightly lower productivity targets aimed at true financial break-even might have resulted in broader improvements in provider satisfaction. Put differently, our results suggest that the 25% reduction in visit lengths that we structured in this study came at no significant cost to provider or patient satisfaction, but our results do not preclude the possibility that a more modest visit length reduction or more modest increase in visit volume might increase satisfaction while still maintaining a positive or break-even financial balance after paying scribe costs. Our scribe costs were also higher than they would be in actual practice, as we paid a higher hourly rate than is typical, and we paid for housing and travel for the scribes; thus in real-world implementation, visit volume increases aimed at break-even would be lower.
From the patient perspective, the addition of scribes appeared to raise no clear concerns. Experientially, patients were generally open and welcoming to a scribe being in the room. Statistically, patients did not report a diminished experience despite their visit lengths being shorter, perhaps because the shorter visit came with greater ability for providers to attend to their medical needs. However, patient satisfaction was uniformly quite high throughout the study, and hence, a ceiling effect limited our ability to detect small differences in either direction between the intervention and control groups.
There were several limitations to our study. First, our patient experience survey response rates were relatively low, although well within the range of many patient surveys, and our results may reflect a selection bias for satisfied patients. Second, providers were not randomized to the scribe vs. control groups and were instead recruited on a convenience basis. Improvements in provider experience scores may be influenced by early-adopter bias, although it is less likely that this had any effect on productivity or patient satisfaction scores. Finally, our financial analysis was based on estimates of past performance and not on actual collections from the study period. This may have under- or over-estimated the return on investment.
In summary, we present a study of medical scribes in an academic general internal medicine practice. Scribes supported a greater patient throughput and improved provider perceptions of documentation burden with no decrement in high patient satisfaction. Cumulatively, these results provide reassuring but clearly preliminary evidence that scribes have a place in academic general medicine. As primary care administrative leaders reconfigure provider schedules to accommodate medical scribes, our results also suggest that there may be an ideal balance between fiscal responsibility and provider wellness that maximizes the value of scribes to patients, providers, and the larger healthcare system.
References
Mailey J, Digiovine B, Baillod D, Gnam G, Jordan J, Rubinfeld I. Reducing Hospital Standardized Mortality Rate With Early Interventions. J Trauma Nurs. 2006;13(4):178.
Sinsky C, Colligan L, Li L, et al. Allocation of Physician Time in Ambulatory Practice: A Time and Motion Study in 4 Specialties. Ann Intern Med. 2016;165(11):753. https://doi.org/10.7326/M16-0961
Shultz CG, Holmstrom HL. The Use of Medical Scribes in Health Care Settings: A Systematic Review and Future Directions. J Am Board Fam Med. 2015;28(3):371–381. https://doi.org/10.3122/jabfm.2015.03.140224
Chen MA, Hollenberg JP, Michelen W, Peterson JC, Casalino LP. Patient Care Outside of Office Visits: A Primary Care Physician Time Study. J Gen Intern Med. 2011;26(1):58–63. https://doi.org/10.1007/s11606-010-1494-7
Dyrbye LN, West CP, Burriss TC, Shanafelt TD. Providing Primary Care in the United States: The Work No One Sees. Arch Intern Med. 2012;172(18):1420–1421. https://doi.org/10.1001/archinternmed.2012.3166
Reuben DB, Miller N, Glazier E, Koretz BK. Frontline Account: Physician Partners: An Antidote to the Electronic Health Record. J Gen Intern Med. 2016;31(8):961–963. https://doi.org/10.1007/s11606-016-3727-x
Menon SP. Maximizing Time with the Patient: the Creative Concept of a Physician Scribe. Curr Oncol Rep. 2015;17(12). https://doi.org/10.1007/s11912-015-0484-7
Gellert GA, Ramirez R, Webster SL. The rise of the medical scribe industry: implications for the advancement of electronic health records. Jama. 2015;313(13):1315–1316.
Glossary | TheACMSS.org. https://theacmss.org/glossary/. Accessed October 20, 2017.
Heaton HA, Castaneda-Guarderas A, Trotter ER, Erwin PJ, Bellolio MF. Effect of scribes on patient throughput, revenue, and patient and provider satisfaction: a systematic review and meta-analysis. Am J Emerg Med. 2016;34(10):2018–2028. https://doi.org/10.1016/j.ajem.2016.07.056
Koshy S, Feustel PJ, Hong M, Kogan BA. Scribes in an Ambulatory Urology Practice: Patient and Physician Satisfaction. J Urol. 2010;184(1):258–262. https://doi.org/10.1016/j.juro.2010.03.040
Bank AJ. Annual impact of scribes on physician productivity and revenue in a cardiology clinic. Clin Outcomes Res. 2015:489. https://doi.org/10.2147/CEOR.S89329
Earls ST, Savageau JA, Begley S, Saver BG, Sullivan K, Chuman A. Can scribes boost FPs’ efficiency and job satisfaction? J Fam Pract. 2017;66(4):206–214.
Pozdnyakova A, Laiteerapong N, Volerman A, et al. Impact of Medical Scribes on Physician and Patient Satisfaction in Primary Care. J Gen Intern Med. 2018. https://doi.org/10.1007/s11606-018-4434-6
Team Documentation - STEPS Forward. STEPSforward.org. https://www.stepsforward.org/modules/team-documentation. Accessed October 21, 2017.
Probst JC, Greenhouse DL, Selassie AW. Patient and physician satisfaction with an outpatient care visit. J Fam Pract. 1997;45(5):418–425.
Gidwani R, Nguyen C, Kofoed A, et al. Impact of Scribes on Physician Satisfaction, Patient Satisfaction, and Charting Efficiency: A Randomized Controlled Trial. Ann Fam Med. 2017;15(5):427–433. https://doi.org/10.1370/afm.2122
Yan C, Rose S, Rothberg MB, Mercer MB, Goodman K, Misra-Hebert AD. Physician, Scribe, and Patient Perspectives on Clinical Scribes in Primary Care. J Gen Intern Med. 2016;31(9):990–995. https://doi.org/10.1007/s11606-016-3719-x
Acknowledgments
The authors would like to thank the leadership team, faculty, staff, and patients of HCA and BIDMC for making this project possible as well as the Linde Family Fellowship in Primary Care Leadership team for their mentorship, guidance, and support during the design and implementation of this project.
Funding
The Linde Family Institute for Primary Care and the Beth Israel Deaconess Division of General Internal Medicine
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Prior Presentation
An earlier version of the manuscript was presented as a short abstract at the 2018 Society for General Internal Medicine annual meeting.
Rights and permissions
About this article
Cite this article
Heckman, J., Mukamal, K.J., Christensen, A. et al. Medical Scribes, Provider and Patient Experience, and Patient Throughput: a Trial in an Academic General Internal Medicine Practice. J GEN INTERN MED 35, 770–774 (2020). https://doi.org/10.1007/s11606-019-05352-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-019-05352-5