Abstract
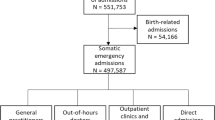
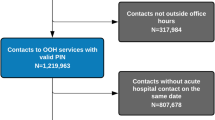
Out of hours (OOH) doctors can have an important gate-keeping role over the access to the emergency department (ED), but the outcome and the quality of their ED referrals have been poorly studied. We aimed to investigate the outcome of patients referred to ED from OOH service and the determinants of admission or short-stay dispositions. We collected retrospectively data about referrals to ED from a local OOH service in the north-east of Italy using the OOH paper register and the ED electronic database, over the period of 01/10/2012 to 31/03/2013. Out of 5217 patients accessing the OOH service, 408 referrals were included in our analysis. 45.3% (185) of the referrals were admitted to hospital or the short-stay unit, 26 patients (=6.4%) were discharged as non-urgent outgoing codes after no specialist consultation or test, suggesting inappropriate referrals, and, of the remaining 197 (=48%), only 10 did not undergo any investigation or consultation. Significant determinants of admission were: age ≥65 years (OR = 2.619; 95% CI 1.528–4.491, p < 0.0001), domiciliary examination (OR = 2.168; 95% CI 1.353–3.476, p = 0.001), nursing home/palliative care setting (OR = 2.563; 95% CI 1.228–5.351, p = 0.012) and OOH triage code, ranging from an OR of 7.47 (95% CI 3.028–18.433) for minor urgencies to an OR of 26.835 (95% CI 6.761–106.508, p < 0.0001) for emergencies, in comparison to no urgent codes. OOH service seems to play an effective gate-keeping role limiting ED access. Determinants of admission to hospital suggest some simple interventions that could improve the adequacy of ED referral from OOH service.

Similar content being viewed by others
References
Morris S, Boyle A, Beniuk K, Robinson S (2012) Emergency department crowding: towards an agenda for evidence-based intervention. Emerg Med J 29:460–466. doi:10.1136/emj.2010.107078
Uscher-Pines L, Pines J, Kellermann A, Gillen E, Mehrotra A (2013) Deciding to visit the Emergency Department for non-urgent conditions: a systematic review of the literature. Am J Manag Care 19:47–59
O’Kelly FD, Teljeur C, Carter I, Plunkett PK (2010) Impact of a GP cooperative on lower acuity emergency department attendances. Emerg Med J 27:770–773. doi:10.1136/emj.2009.072686
Wong WB, Edgar G, Liddy C, Vaillancourt C (2009) Can after-hours family medicine clinics represent an alternative to emergency departments? Survey of ambulatory patients seeking after-hours care. Can Fam Phys 55(1106–1107):e4
Grol R, Giesen P, van Uden C (2006) After-hours care in the United Kingdom, Denmark, and the Netherlands: new models. Health Aff 25:1733–1737. doi:10.1377/hlthaff.25.6.1733
O’Malley AS (2013) After-hours access to primary care practices linked with lower emergency department use and less unmet medical need. Health Aff 32:175–183. doi:10.1377/hlthaff.2012.0494
van der Straten LM, van Stel HF, Spee FJM et al (2012) Safety and efficiency of triaging low urgent self-referred patients to a general practitioner at an acute care post: an observational study. Emerg Med J 29:877–881. doi:10.1136/emermed-2011-200539
Dale J, Green J, Reid F et al (1995) Primary care in the accident and emergency department: II. Comparison of general practitioners and hospital doctors. BMJ 311:427–430
Rossdale M, Kemple T, Payne S, Calnan M (2007) An observational study of variation in GPs’ out-of-hours emergency referrals. Br J Gen Pract 57:152–154
Calnan M, Payne S, Kemple T et al (2007) A qualitative study exploring variations in GPs’ out-of-hours referrals to hospital. Br J Gen Pract 57:706–713
Buja A, Toffanin R, Rigon S et al (2015) Out-of-hours primary care services: demands and patient referral patterns in a Veneto region (Italy) Local Health Authority. Health Policy (New York). doi:10.1016/j.healthpol.2015.01.001
Scapinello P, Posocco A, De Ronch I et al (2016) Predictors of Emergency Department referral in patients using out-of-hours primary care services. Health Policy (New York). doi:10.1016/j.healthpol.2016.07.018
Bezzina AJ, Smith PB, Cromwell D, Eagar K (2005) Primary care patients in the emergency department: who are they? A review of the definition of the “primary care patient” in the emergency department. Emerg Med Australas 17:472–479. doi:10.1111/j.1742-6723.2005.00779.x
Buja A, Toffanin R, Rigon S et al (2016) Determinants of out-of-hours service users’ potentially inappropriate referral or non-referral to an emergency department: a retrospective cohort study in a local health authority, Veneto Region, Italy. BMJ Open 6:e011526. doi:10.1136/bmjopen-2016-011526
Tosato F (2013) Triage. Regolamentazione dei sistemi di emergenza sanitaria, Piccin
Cohen J (1960) A coefficient of agreement for nominal scales. Educ Psychol Meas 20:37–46. doi:10.1177/001316446002000104
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174. doi:10.2307/2529310
Burman RA, Zakariassen E, Hunskaar S (2014) Management of chest pain: a prospective study from Norwegian out-of-hours primary care. BMC Fam Pract 15:1–7. doi:10.1186/1471-2296-15-51
Mcdermott C, Coppin R, Little P, Leydon G (2012) Hospital admissions from nursing homes: a qualitative study of GP decision making Br J Gen Pract 62:e538–e545
De Korte-verhoef MC, Pasman HRW, Schweitzer BPM et al (2012) End-of-life hospital referrals by out-of-hours general practitioners: a retrospective chart study. BMC Fam Pract 13:1. doi:10.1186/1471-2296-13-89
Acknowledgements
We are very grateful to Dr. John O’ Malley for the contribution to the English language editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Statement of human and animal rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
All patients enrolled in the study have read and signed the informed consent.
Funding
No source of funding.
Data availability
The datasets analysed during the current study are available from the corresponding author on request.
Rights and permissions
About this article
Cite this article
Posocco, A., Scapinello, M.P., De Ronch, I. et al. Role of out of hours primary care service in limiting inappropriate access to emergency department. Intern Emerg Med 13, 549–555 (2018). https://doi.org/10.1007/s11739-017-1679-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-017-1679-8