Abstract
Purpose of review
Peptic ulcer disease (PUD) is a recognized complication of non-steroidal anti-inflammatory drugs (NSAIDs). Stress ulcers are a concern for intensive care unit (ICU) patients; PUD is also an issue for patients taking anticoagulation. Helicobacter pylori test and treat is an option for patients starting NSAID therapy, and proton pump inhibitors (PPIs) may reduce PUD in NSAID patients and other high-risk groups.
Recent findings
There are a large number of trials that demonstrate that Helicobacter pylori eradication reduces PUD in NSAID patients. PPI is also effective at reducing PUD in this group and is also effective in ICU patients and those on anticoagulants. The effect is too modest for PPI to be recommended in everyone, and more research is needed as to which groups would benefit the most. Increasing age, past history of PUD, and comorbidity are the most important risk factors.
Summary
H. pylori test and treat should be offered to older patients starting NSAIDS, while PPIs should be prescribed to patients that are at high risk of developing PUD and at risk of dying from PUD complications.
Similar content being viewed by others
Introduction
Upper gastrointestinal (GI) bleeding is a major health problem, and mortality from this problem has remained relatively unchanged for the last 50 years [1,2,3]. The apparent stability of a 5–12% in-patient 30-day mortality rate hides significant changes in the epidemiology and management of the condition. Major advances have been made in the management of upper gastrointestinal bleeding including the routine use of proton pump inhibitor therapy after a peptic ulcer bleed which improves outcomes and probably reduces mortality [4]. Endoscopic therapy also improves the outcomes of peptic ulcer and variceal bleeding [5]. The age-adjusted rates of peptic ulcer (PU) bleeding have fallen globally over the last 20 years largely due to the falling prevalence of Helicobacter pylori (H. pylori) [6, 7], but a modest contribution may relate to the increasing use of acid suppression in the community [8]. These positive factors have been balanced by the fluctuating use of non-steroidal anti-inflammatory drug (NSAID) [9] and by the increased use of antiplatelet [10] and anticoagulant therapy [11] over time. Furthermore, the absolute numbers of patients with peptic ulcer bleeding are not falling as dramatically as might be expected due to populations living longer with more comorbidities, which are a major risk factor for both PU bleeding incidence [12] and death [13].
Given that PU bleeding remains an important problem, it is helpful to develop strategies that will prevent this complication particularly as antiplatelet and anticoagulation therapy continue to rise [14]. There have been recent guidelines [15, 16] on non-variceal upper gastrointestinal bleeding, but these have predominantly focused on management of the problem when it occurs rather than preventing the complication from happening in the first place. The main approaches to prevent peptic ulcer bleeding are H. pylori screening and treating those that are positive, long-term proton pump inhibitor (PPI), or H2 receptor antagonists (H2RA) therapy. H2RA therapy is less effective than PPI [17] and will not be considered further in this review. In those taking NSAIDs, there are the additional approaches of replacing them with cyclooxygenase-2 (COX-2) inhibitors or adding prostaglandin analogues. None of these strategies will be cost-effective if used in the general population, and most guidelines would recommend that these interventions should only be used in high-risk groups [18]. This article will therefore evaluate risk factors for PU complications such as age, NSAID use, concomitant antiplatelet therapy, anticoagulant therapy, patients admitted to intensive care, and those with severe comorbidities [19]. We will then summarize the evidence for the efficacy of H. pylori eradication, PPI therapy, COX-2 inhibition, and prostaglandin analogues in preventing peptic ulcer bleeding and focus on which high-risk groups these approaches could be recommended.
High-risk groups for peptic ulcer complications
Increasing age
The most important determinant of PU complication population attributable to risk is increasing age. The risk of PU complication is 10-fold higher than those over the age of 60 years compared to younger age groups [20]. The vast majority of deaths from PU complications also occur in older age groups with a 50-fold increase in mortality in those over 60 compared to those less than 60 years old [20]. While mortality from PU complications in those under that age of 60 years is very rare, this cut off is somewhat arbitrary. The risk of PU complications is still modest in a 60-year-old but steadily increases with advancing age with a roughly two-fold increase in incidence with every decade [21]. Many risk factors increase with age, and it is difficult to evaluate age separate from other risk factors such as increasing prevalence of H. pylori, polypharmacy, and comorbidity. Nevertheless, it is likely that age is an important independent risk factor for PU complications. The message for the clinician is that gastroprotection is unlikely to be cost-effective in younger age groups and should mainly be considered in those over the age of 60 years. In those over the age of 60, the threshold to offer gastroprotection should decrease as age increases with a particular consideration given to those over the age of 80 years [21].
Non-steroidal anti-inflammatory drugs
The potential for NSAIDs to cause peptic ulcer disease is well known. The analgesic effect of NSAIDs is mediated through reducing prostaglandin synthesis by inhibiting cyclooxygenase (COX) enzymes. There are two COX isoenzymes; COX-1 is present in most cells whereas COX-2 is present in only a few tissues and is induced by inflammation [22]. The gastrointestinal toxicity of NSAIDs is mediated by COX-1, and the reduction in GI prostaglandin caused by this isoform leads to loss of cytoprotection and increased risk of peptic ulceration. All traditional NSAIDS have a mixture of COX-1 and COX-2 inhibitor activity, but the proportions differ, and this is the main reason their gastrointestinal toxicity also varies [23]. The least toxics are ibuprofen and diclofenac with relative risks (RR) of around two followed by naproxen with RR of four, and the most toxics are piroxicam and ketoprofen with RR of 8 for the development of peptic ulcer disease [24, 25]. Low-dose acetylsalicylic acid (ASA) also has an increased risk of peptic ulcer complications with a RR of approximately 1.5 [26]. A modeling study [27] from RCT and cohort study data suggested that 1:1200 to 1:2000 chronic NSAID users will die from peptic ulcer complications attributable to the drug.
Antiplatelet therapy
Adenosine diphosphate-receptor inhibitors such as clopidogrel are typically used after acute coronary syndromes and following percutaneous coronary stenting as they reduce the risk of future coronary events at least over the next year [28]. The seminal study [28] that reported the benefit of dual antiplatelet therapy with clopidogrel and ASA in acute coronary syndromes also found that 1.3% developed GI bleeding over the next 9 months. The pathways that ASA causes gastrointestinal mucosal damage are well described, as with all NSAIDs, but the mechanism by which antiplatelet therapy leads to peptic ulcer bleeding is less clear. Inhibition of platelet activity in a peptic ulcer that is already hemorrhaging will aggravate the problem and may lead to more peptic ulcers presenting with bleeding that would otherwise have remained “silent.” Platelet-derived growth factors promote angiogenesis, and this is important in ulcer healing [29]. Disruption of these growth factors by clopidogrel may impair peptic ulcer healing and lead to more complications. A population-based cohort [30] estimated the number needed to harm ranged between 30 and 60 for a gastrointestinal hemorrhage within the first 12 months of clopidogrel compared to those not taking this drug. This excess could be related to bias and confounding factors inherent with database studies, but a systematic review [26] of RCTs supported this finding, and patients on dual antiplatelet therapy had almost twice the rate of gastrointestinal bleeding compared to those taking ASA alone.
Anticoagulant therapy
Anticoagulants are commonly used to prevent thromboembolic events in patients with venous thromboembolism, atrial fibrillation, or mechanical heart valves. Clinicians and patients are well aware of the risk of bleeding from vitamin K antagonist anticoagulants such as warfarin. The risk of peptic ulcer bleeding is remarkably difficult to quantify as there are no RCTs evaluating the risks of warfarin compared to placebo and there are remarkably few robust epidemiological studies. Most older studies follow cohorts of patients taking warfarin with no comparator group [31] and suggest a large risk. It is generally believed that traditional views of the GI bleeding risks of warfarin are overestimated [32] and more contemporary assessments of risk support a more modest increased risk [33]. A systematic review [34] of randomized trials comparing anticoagulation with ASA in atrial fibrillation found that major bleeding adverse events were more common in the anticoagulation group (OR = 1.45; 95% CI = 0.93 to 2.27). This was all bleeding events and was not limited to peptic ulcer bleeding, but if we assume that this also reflects upper GI bleeding and factor in that ASA alone also causes an increased risk of bleeding [26], the overall risk from vitamin K antagonists is approximately increased three-fold.
More recently the non-vitamin K antagonist oral anticoagulants (NOACs) have been developed and shown to be more efficacious than warfarin in many settings, particularly related to atrial fibrillation [35]. As a result, NOACs have overtaken the prescription of vitamin K antagonists for atrial fibrillation and deep vein thrombosis in the USA and several other countries [36]. NOACs also cause less intracranial bleeding than vitamin K antagonist but are associated with greater risk of GI bleeding [35]. This meta-analysis of RCTs [35] is considering all NOACs together, and there are significant differences in risk of GI bleeding between drugs in this class. One database study [37] suggested that apixaban was associated with less GI bleeding than dabigatran or rivaroxaban although another found dabigatran was associated with less upper GI bleeding [38]. Interestingly these database studies found similar rates of GI bleeding with NOACs compared to vitamin K antagonists. This is in contrast to RCT data, and this may relate to confounding factors or may relate to patients outside of RCTs having their coagulation less rigorously monitored. The development of NOACs has lowered the threshold at which anticoagulation is considered, and they are being used for ever wider indications [39]. This emphasizes the need to offer gastroprotection in patients taking anticoagulation if they are at a high risk of PU bleeding. Defining high-risk groups is a challenge but there is RCT evidence [39] that adding a NAOC to ASA doubles the risk compared to ASA alone. There is also cohort evidence [40] that adding warfarin to clopidogrel triples the bleeding risk.
Corticosteroid therapy
Corticosteroids have a wide range of actions including profound immunomodulatory effects. They are used in a wide range of inflammatory and auto-immune conditions [41], and their adverse event profiles such as osteoporosis, obesity, mood disorder, diabetes mellitus, and risk of infection are well known. Corticosteroids also delay wound healing, so it is logical that they may also inhibit peptic ulcer healing and be associated with increased risk of ulcer complications. Clinicians are well aware of this putative risk and often provide patients with ulcer prophylaxis [42]. The RCT evidence that they cause peptic ulcer complications is however less clear. A systematic review of RCTs [43] did find an approximately 40% increase in risk peptic ulcer bleeding or perforation in those taking corticosteroids. However, the statistically significant effect was only seen in hospitalized patients and with events only occurring in 0.1% of ambulatory patients. These data suggest that the main risk is in patients with other risk factors for peptic ulcer complications, particularly those admitted to hospital, and there is no need to routinely provide gastroprotection to those in the community. The main focus should be on limiting the duration of therapy given the other adverse events related to corticosteroids rather than focusing on gastroprotection.
Selective serotonin reuptake inhibitors
Selective serotonin reuptake inhibitors (SSRIs) are the most commonly prescribed antidepressant [44] and have been advocated for a variety of psychiatric and medical conditions [45]. They have a favorable adverse event profile compared to more traditional antidepressants [46], but concerns have been raised regarding the risk of GI bleeding [47]. SSRIs decrease platelet serotonin, and this can result in reduced platelet aggregation [48]. SSRIs also increase gastric acid production, which could lead to a greater propensity to develop peptic ulceration [49]. An initial UK database study [50] did suggest a threefold increase in GI bleeding in those taking an SSRI compared to controls, and this was supported by another cohort study [51]. There have been no RCTs evaluating GI bleeding as an outcome, but further observational data has accrued. A systematic review [52] identified 15 case-control studies involving almost 4000 participants and found an increased risk of upper GI bleeding with SSRI therapy compared to controls with an odds ratio (OR) of 1.66 (95% confidence intervals (CI) = 1.44 to 1.92). The systematic review [52] also identified four cohort studies, and the increased risk was similar (OR = 1.68; 95% CI = 1.13 to 2.50). The number needed to harm over 1 year varied between 3177 in a low-risk Dutch population and 881 in a higher risk US population [42]. The systematic review [52] also evaluated the impact of NSAIDs on the risk of upper GI bleed and found at least an additive effect. The risk of upper GI bleeding in patients taking SSRIs alone was 1.66, in those taking NSAID alone it was 2.8, and in those taking both drugs the OR was 4.25. The number needed to harm for those taking both NSAIDs and SSRIs was 645 for a low-risk population and 179 for a higher risk US population [52].
These results could be due to bias or residual confounding as they relate to observational data, but these findings are supported by a Hong Kong study that attempted to reduce this concern [53]. This study evaluated 3358 SSRI users and 57,906 non-users and only included patients that had H. pylori eradication therapy. This approach makes the population more homogeneous, and they further reduced the possibility of confounding by conducting a propensity match analysis. The propensity-matched analysis found patients taking SSRI had a hazard ratio of 1.95 (95% CI = 1.41 to 2.71) for developing upper GI bleed compared to non-users [53].
Helicobacter pylori
H. pylori is the leading cause of peptic ulcer disease worldwide [54, 55], and a proportion of both gastric and duodenal ulcers caused by this infection will go on to develop complications. A systematic review of observational studies suggested H. pylori is associated with a two-fold increase in peptic ulcer bleeding [56]. There also appears to be an interaction between NSAIDs and H. pylori as the same systematic review [56] found an approximately four-fold increased risk of developing peptic ulcer bleeding in those taking NSAIDS and a 6-fold increase in patients where both factors were present. A further systematic review [57] also found a two-fold increase in upper gastrointestinal bleeding in ASA users infected with H. pylori compared to those that were not infected. The number needed to treat varied between 100 and 1000 depending on the underlying risk of peptic ulcer disease in the population [57].
Comorbidity
Serious comorbidity is associated with peptic ulcer bleeding although definitions of comorbidity vary between studies [7]. Patients admitted to the intensive care unit (ICU) exemplify the risk facing patients with severe stress and comorbidity with around 3% developing significant GI bleeding [58], and this is associated with length of stay severity of underlying illness [59]. Various scoring systems [60, 61] that evaluate risk of mortality from upper GI bleeding include comorbidity as part of the calculations. A systematic review of death from peptic ulcer bleeding [62] found that mortality was significantly higher in those with comorbidity than those without. In particular those with malignancy had a 6-fold, those with renal disease a 5-fold, and those with hepatic disease a 4-fold increased risk of mortality [62]. Respiratory and cardiac disease were each associated with a two-fold risk of dying from peptic ulcer bleed and diabetes mellitus a relative risk of 1.6 [62]. It is important to note that only three of the 16 studies identified in this review were low risk of bias so the quality of the evidence is low, but nevertheless the impact of comorbidity seems to be important, and there is less research on this than many other risk factors for peptic ulcer bleeding.
Previous history of peptic ulcer disease
Past history of peptic ulcer disease is a strong risk factor for future peptic ulcer although the impact is less strong after successful H. pylori eradication [63]. There is a paucity of data on the risk of developing complicated peptic ulcer in comparison with population-based controls. Systematic review data [64] suggest that in patients taking NSAIDs, a previous history of peptic ulcer increases the risk of future peptic ulcer two to three-fold, and this increases for 4–6 fold for a past history of bleeding peptic ulcer. This is also supported by subgroup analyses of randomized controlled trials [65]. Patients with a previous history of peptic ulcer prescribed oral anticoagulants have a doubling of their risk of having a GI bleed over a 10-year follow-up [66].
Approaches to preventing peptic ulcer complications
There are a number of risk factors for developing peptic ulcer disease complications, but the main focus of research has related to preventing NSAID-related peptic ulcer complications. This is understandable as this causes one of the highest increases in risk. The strategies that reduce NSAID-related bleeding are adding PPI therapy, substituting for a COX-2 inhibitor, or adding a prostaglandin analogue. The other approach is screening and treating for H. pylori, and this is the only approach that could be considered for patients other than those taking NSAIDs.
Helicobacter pylori screening and treatment
Seven days of eradication therapy can heal most patients with H. pylori-positive PUD [67], and treating the infection also dramatically reduces future ulcer recurrence [63]. This also applies to bleeding peptic ulcer as a systematic review of 7 RCTs involving 578 infected bleeding patients reported that H. pylori eradication was more effective than anti-secretory therapy in preventing future bleeding recurrence [68]. The recurrence rate was 20% in the anti-secretory group and 3% in the H. pylori eradication group with a number needed to treat of seven. Most guidelines [15, 16] therefore recommend testing for H. pylori in those with bleeding PUD and treating those infected. Randomized controlled trials have shown that population H. pylori screening and treatment reduces the incidence of peptic ulceration in the community [69, 70]. The impact on peptic ulcer complications in the general population is less certain, however, as these events are too rare for randomized trials to be powered to detect an impact on this outcome. The rare events observed in these trials highlight that testing for H. pylori is unlikely to be cost-effective in all groups and any population strategy to screen and treat cannot be instituted on the basis of reduced peptic ulcer complications. Population H. pylori screening and treatment is advocated in countries that have a high incidence of gastric adenocarcinoma [71, 72] as systematic reviews of randomized controlled trials have shown that this reduced risk of gastric adenocarcinoma [73, 74]. Population H. pylori screening and treatment could increase both the length and quality of life, and it has been estimated that almost 9 million disability-adjusted life years could be gained globally [74, 75]. This estimate just focuses on reduction in gastric cancer, and if prevention of peptic ulcer complications was considered, then the disability life years gained could be even higher. Furthermore, a randomized controlled trial has suggested that H. pylori population test and treat could be cost neutral due to the reduction in dyspepsia in the population [76,77,78]. Guidelines do not support population H. pylori screening and treatment in North America [79], but the other benefits that could accrue from this approach suggest the clinician should have a low threshold for instituting this strategy when considering patients that may be at risk of developing PU complications. For example, patient taking only low-dose ASA who are H. pylori positive may benefit from eradication therapy as one study reported that infected patients who had an ASA-related PU bleed given eradication therapy had a similar risk for future bleeding as patients who were ASA naïve that had not had a bleed [80]. Similarly, a systematic review of RCTs [81] reported that patients allocated to H. pylori eradication had an almost 60% reduction in incidence of PUD compared to infected NSAID patients in the control group. As this involves one of course of antibiotics for 2 weeks rather than long-term treatment with acid suppressive agents, this could be a very cost-effective approach [82] at preventing NSAID-related ulceration, and guidelines are now recommending this strategy [79, 83]. However, H. pylori eradication is not as effective as PPI therapy in patients on long-term NSAID therapy [81], so this strategy is not sufficient for some patient groups.
Proton pump inhibitor therapy
NSAIDs reduce gastric prostaglandin production and loss of mucosal defenses leading to an increased risk of PUD [84]. The main reason that mucosal protection is necessary is the highly acid environment of the stomach. Blocking acid production should reduce the risk of PUD even if there is NSAID-mediated loss of mucosal protection. Clinical data support this hypothesis with a systematic review [85] of 18 RCTs involving over 10,000 participants demonstrating that PPIs reduced PUD bleeds by approximately 80% compared to controls although the effect was less marked in patients who were already taking NSAID therapy long term. Overall the number needed to treat (NNT) was around 100 in these trials although this was heavily dependent on the underlying risk of the population. PPIs also prevented symptomatic and endoscopic ulcers in patients taking NSAIDs with an NNT of 20 and 5, respectively [85, 86]. A systematic review [87, 88] of 5 RCTs involving over 5000 participants also reported that PPIs are effective in reducing PU bleeding related to clopidogrel-based antithrombotic therapy. There was a 66% reduction in PU bleed in patients allocated to PPI compared to placebo or famotidine with an NNT of 60 [88].
Research on the gastroprotective role of PPI therapy has focused on patients taking NSAID and/or ASA. There are a growing number of patients on anticoagulation therapy [36], and these patients are at increased risk of PU bleed [37]. This was evaluated as part of the Cardiovascular Outcomes for People Using Anticoagulant Strategies (COMPASS) trial [39]. Participants were randomized to rivaroxaban 2.5 mg twice daily with aspirin 100 mg once daily, rivaroxaban 5 mg twice daily alone, or aspirin 100 mg once daily alone to evaluate cardiovascular death, stroke, or myocardial infarction in these groups [39].This is a 3-by-2 partial factorial RCT as those that were not on a PPI were also randomized to pantoprazole 40 mg or placebo [89••]. A total of 17,598 patients were randomized to the PPI or placebo, and there was no statistically significant difference in the primary outcome of the trial, which was clinically significant upper GI events [89••]. There was a 50% reduction in the gastroduodenal bleeding in the PPI arm, but events were low and the NNT = 1770 after 3 years of PPI use. The definitions of PUD and PU bleeding were very stringent, and this may have resulted in the NNT being so high. A post hoc analysis was therefore conducted relaxing definitions, and this did result in a 50% reduction in bleeding PUD bleed, and a similar reduction in uncomplicated PUD as well as a 66% reduction in gastric erosions in the PPI group. Even when these outcomes were combined, the NNT was still around 500 [89••]. Furthermore, the main benefit of PPI therapy was seen in the ASA alone group emphasizing PPIs have little impact in patients taking anticoagulants alone. Evidence therefore suggests that any benefit of PPIs relates to patients taking NSAID or ASA.
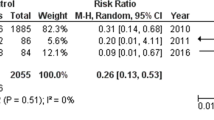
The final group to consider are patients admitted to the ICU as these patients are at increased risk of bleeding from upper gastrointestinal stress ulceration [58, 59]. Systematic reviews [90, 91] of 19 RCTs involving over 2000 ICU patients found that PPI therapy reduced overt GI bleeding by 50% with no impact on length of stay, pneumonia, or mortality. PPIs were superior to H2RA in these reviews although this is disputed by a network meta-analysis [92••] of 43 RCTs involving over 10,000 patients evaluating clinically important upper GI bleeding as an outcome. This review concluded both PPIs and H2RAs reduced GI bleeding, and PPIs were possibly superior, but the 95% CI were wide (OR = 0.58; 95% CI 0.29 to 1.17). This review highlighted that either PPI or H2RA were probably not beneficial in low-risk patients and this intervention should be reserved for those at high risk.
The benefits of PPI therapy in preventing PU bleeding should be weighed against the harm of this approach. Patients need to take PPI therapy for the duration of risk which may be life-long in the case of ASA users. Previously this would have been a significant expense, but as most PPIs are now available generically in most countries, the costs have reduced significantly. PPI therapy is also very safe in the short term [93], but concerns have been raised around the long-term adverse effects associated with these drugs [94]. PPIs have been associated with pneumonia [95], bone fracture [96], enteric infections [97], cardiovascular events [98], chronic kidney disease [99], dementia [100], gastric cancer [101], and even all-cause mortality [102]. The list of concerns increases with each passing year, and the latest harms that have been highlighted are an increased risk of renal calculi [103, 104] and risk of COVID-19 [105]. The problem with all of these associations is that they are based on observational data, usually related to administrative databases. All of these studies have shown that sicker patients tend to be prescribed PPI therapy and comorbidities are a strong risk factor for developing other diseases [106]. It is possible that being prescribed PPI therapy is a good marker for comorbidity and all of these harms relate to residual confounding [106]. To evaluate this possibility, the RCT evaluating PPI in patients taking anticoagulation and/or ASA [89••] described above also prospectively collected information on adverse events [107•]. In over 53,000 patient years of follow up, there was no difference in risk of pneumonia, fracture, chronic kidney disease, dementia, myocardial infarction, gastrointestinal cancers, and all-cause mortality between the PPI and placebo groups [107•]. The PPI group had slightly more enteric infections than those taking placebo, but the number needed to harm was over 900 for each year of PPI therapy. This trial followed patient for 3 years, and it is possible that adverse events may take longer to accrue, but there was no divergence on the curves over time in the RCT [107•]. Furthermore, an RCT also found no adverse events in PPI arm compared to surgery in reflux patients over 12 years [108] although this trial was underpowered. Finally, there was actually a reduction in mortality in the high-dose PPI arm of a Barrett’s esophagus trial comparing esomeprazole 20 mg versus 40 mg bid given over a mean of 9 years in over 2500 patients [109]. There are also concerns that PPI may interact with clopidogrel reducing efficacy [110•] and this could not be addressed in the COMPASS trial as patients had to discontinue this drug. A systematic review of RCTs [87, 88] did not find any difference in cardiovascular events in the PPI arm compared to the placebo/famotidine arms in patients taking clopidogrel suggesting that the results of observational data probably relate to residual confounding. These data suggest that the benefits of PPI therapy outweigh any putative risk provided the appropriate patients are selected for gastroprotection.
Cyloxgenase-2 inhibitors
The gastrointestinal adverse effects of NSAIDs largely relate to the COX-1 activity of the drug, while the analgesic effects of NSAIDs relate to COX-2 inhibition. COX-2 selective inhibitors were therefore developed on the principle that these drugs could provide similar analgesic properties to traditional NSAIDs without the gastrointestinal events [111]. Systematic reviews of RCTs confirmed this hypothesis with COX-2 inhibitors having a similar efficacy profile [112] but with a 70% reduction in endoscopic ulcers [113] and a 60% reduction in PU bleed and PU complications [113]. COX-2 inhibitors were initially used widely to protect against NSAID-related GI injury, but enthusiasm for this approach waned once it became apparent from RCTs [114, 115] that the risk of cardiovascular events was increased from these drugs. A systematic review [116] of 280 RCTs comparing NSAIDs/Cox-2 inhibitor with placebo and 474 RCTs comparing NSAIDs with another NSAID/COX-2 inhibitor confirmed that COX-2 inhibitors increased the risk of cardiovascular events by about 33% and this outweighed any benefits in terms of reduction of PU complications. An increase in cardiovascular event risk was also seen with NSAIDs such as diclofenac and ibuprofen, and the impact seemed as great as with COX-2 inhibitors [116]. In contrast, naproxen was not associated with an increased risk of cardiovascular events, suggesting this was a safer NSAID to use [116]. These data raise the question of whether any NSAID other than naproxen is safe to use in the long term as a 33% increase in cardiovascular disease will outweigh any improvement in quality of life for most patients. Furthermore, another systematic review of RCTs [117] suggested COX-2 inhibitors were associated with an increased risk of dementia, highlighting there may be other risks to taking these drugs long-term.
Prostaglandin analogues
Another approach to gastroprotection is to replace the upper gastrointestinal deficiency in prostaglandin caused by NSAIDs with a prostaglandin analogue. Misoprostol, a synthetic prostaglandin E1 analogue, dramatically reduces endoscopic ulcers in a systematic review of 22 RCTs involving almost 6000 patients taking NSAIDs with an NNT of 10 [85]. There was early promise [65] that this would translate into a reduction in PU complications, but this was not supported by a systematic review of three RCTs involving almost 9000 patients, where there was no statistically significant reduction in PU bleeding [85]. The use of misoprostol is also limited by adverse events such as diarrhea with up to 20% patients withdrawing because of adverse events [118]. This can be mitigated by lowering the dose [118], but it remains a significant problem when used for long-term prophylaxis. Prostaglandin analogues therefore cannot be recommended for gastroprotection routinely in patients taking NSAIDs. There may be selected patients where this might be the appropriate drug. For example, RCT data suggest that misoprostol may reduce NSAID-related small bowel ulcers detected by video capsule endoscopy [119]. Whether this translates to improvement in clinical outcomes remains to be determined, but this may be an option for patients with predominantly small bowel ulcer problems that cannot discontinue NSAIDs.
Recommendations for gastroprotection
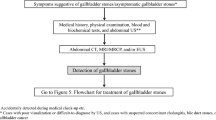
The above evidence provides a framework to selecting which patients should receive gastroprotection. In general, these should be reserved for patients over the age of 60 years taking NSAIDs or those being admitted to ICU. Even in these groups, the risk is not sufficiently high to warrant gastroprotection to everyone [92••]. Ideally what is required is a validated risk calculator that gives the absolute risk of developing peptic ulcer disease over a given period of time similar to those used to determine risk of cardiovascular disease [120]. Patients starting long-term NSAID or low-dose ASA therapy should all routinely be screened for H. pylori, and those infected should receive eradication therapy with regimens that follow latest guidelines [79, 121]. This will reduce PU complications but will also have added benefits in reducing future dyspepsia and future gastric cancer risk. As this is a one-off treatment, this is likely to be cost-effective. For those over 60 years of age taking long term NSAIDs, naproxen should be the drug of choice due to the favorable cardiovascular risk profile. Additional risk factors should be ascertained according to the scoring system outlined in Table 1. Those that have 6 points or more for naproxen or 8 points for low-dose ASA (as the underlying risk of developing PU complication is lower than for naproxen) should be offered long-term PPI therapy with careful discussion of the risks and benefits. For patients admitted to ICU, additional risk factor should also be ascertained as determined by a systematic review [122] that identified 8 observational studies involving over 116,000 ICU patients. Patients with chronic liver disease and/or coagulopathy should be given prophylaxis with PPI therapy during their hospital admission [122]. Similarly, those that need mechanical ventilation and are also in shock may benefit from PPI therapy [122]. Those that are discharged should have their PPI discontinued if there is no indication for continued therapy [123].
Conclusions
There is a wealth of RCT evidence on the benefits of H. pylori eradication and PPI therapy to prevent PU complications in patients taking NSAID. There is also RCT evidence on the benefits of PPI therapy in patients taking anticoagulation and for ICU patients. It is clear from these trials that these interventions are effective, but high-risk groups need to be identified, and this should be the focus of future research.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Laine L, Yang H, Chang SC, Datto C. Trends for incidence of hospitalization and death due to GI complications in the United States from 2001 to 2009. Am J Gastroenterol. 2012;107:1190–5.
van Leerdam ME, Vreeburg EM, Rauws EA, et al. Acute upper GI bleeding: did anything change? Time trend analysis of incidence and outcome of acute upper GI bleeding between 1993/1994 and 2000. Am J Gastroenterol. 2003;98:1494–9.
Wang YR, Richter JE, Dempsey DT. Trends and outcomes of hospitalizations for peptic ulcer disease in the United States, 1993 to 2006. Ann Surg. 2010;251:51–8.
Leontiadis GI, Sharma VK, Howden CW. Systematic review and meta- analysis of proton pump inhibitor therapy in peptic ulcer bleeding. BMJ. 2005;330:568–70.
Vergara M, Bennett C, Calvet X, Gisbert JP. Epinephrine injection versus epinephrine injection and a second endoscopic method in high-risk bleeding ulcers. Cochrane Database Syst Rev. 2014;(10):Art. No.: CD005584. https://doi.org/10.1002/14651858.CD005584.pub3.
Sung JJ, Kuipers EJ, El-Serag HB. Systematic review: the global incidence and prevalence of peptic ulcer disease. Aliment Pharmacol Ther. 2009;29:938–46.
Lau JY, Sung J, Hill C, Henderson C, Howden CW, Metz DC. Systematic review of the epidemiology of complicated peptic ulcer disease: incidence, recurrence, risk factors and mortality. Digestion. 2011;84:102–13.
Peery AF, Crockett SD, Murphy CC, Lund JL, Dellon ES, Williams JL, et al. Burden and cost of gastrointestinal, liver, and pancreatic diseases in the United States: update 2018. Gastroenterology. 2019;156:254–72.
Fassio V, Aspinall SL, Zhao X, et al. Trends in opioid and nonsteroidal anti-inflammatory use and adverse events. Am J Manag Care. 2018;24:e61–72.
Karve S, Levine D, Seiber E, Nahata M, Balkrishnan R. Trends in ambulatory prescribing of antiplatelet therapy among US ischemic stroke patients: 2000-2007. Adv Pharmacol Sci. 2012;2012:846163. https://doi.org/10.1155/2012/846163.
Ho KH, van Hove M, Leng G. Trends in anticoagulant prescribing: a review of local policies in English primary care. BMC Health Serv Res. 2020;20:279. https://doi.org/10.1186/s12913-020-5058-1.
Lanas A, Chan FKL. Peptic ulcer disease. Lancet. 2017;390:613–24.
Åhsberg K, Höglund P, Staël von Holstein C. Mortality from peptic ulcer bleeding: the impact of comorbidity and the use of drugs that promote bleeding. Aliment Pharmacol Ther. 2010;32:801–10.
Vaduganathan M, Bhatt DL. Gastrointestinal bleeding with oral anticoagulation: understanding the scope of the problem. Clin Gastroenterol Hepatol. 2017;15:691–3.
Barkun AN, Almadi M, Kuipers EJ, Laine L, Sung J, Tse F, et al. Management of Nonvariceal Upper Gastrointestinal Bleeding: guideline recommendations from the international consensus group. Ann Intern Med. 2019;171:805–22.
Sung JJ, Chiu PW, Chan FKL, et al. Asia-Pacific working group consensus on non-variceal upper gastrointestinal bleeding: an update 2018. Gut. 2018;67:1757–68.
Mo C, Sun G, Wang Y-Z, Lu M-L, Yang Y-S. PPI versus histamine H2 receptor antagonists for prevention of upper gastrointestinal injury associated with low-dose aspirin: systematic review and meta-analysis. PLoS One. 2013;10:e0131558. https://doi.org/10.1371/journal.pone.0131558.
Rostom A, Moayyedi P, Hunt R, Canadian Association of Gastroenterology Consensus Group. Canadian consensus guidelines on long-term nonsteroidal anti-inflammatory drug therapy and the need for gastroprotection: benefits versus risks. Aliment Pharmacol Ther. 2009;29:481–96.
Targownik LE, Metge CJ, Leung S, Chateau DG. The relative efficacies of Gastroprotective strategies in chronic users of nonsteroidal anti-inflammatory drugs. Gastroenterology. 2008;134:937–44.
Thorsen K, Søreide JA, Kvaløy JT, Glomsaker T, Søreide K. Epidemiology of perforated peptic ulcer: age- and gender-adjusted analysis of incidence and mortality. World J Gastroenterol. 2013;19:347–54.
García Rodríguez LA, Ruigómez A, Hasselgren G, Wallander MA, Johansson S. Comparison of mortality from peptic ulcer bleed between patients with or without peptic ulcer antecedents. Epidemiology. 1998;9:452–6.
Drini M. Peptic ulcer disease and non-steroidal anti-inflammatory drugs. Aust Prescr. 2017;40:91–3.
Brune K, Patrignani P. New insights into the use of currently available non-steroidal anti-inflammatory drugs. J Pain Res. 2015;8:105–18.
Lanas A, García-Rodríguez LA, Arroyo MT, Gomollón F, Feu F, et al. Risk of upper gastrointestinal ulcer bleeding associated with selective cyclo-oxygenase-2 inhibitors, traditional non-aspirin non-steroidal anti- inflammatory drugs, aspirin and combinations. Gut. 2006;55:1731–8.
Castellsague J, Riera-Guardia N, Calingaert B, Varas-Lorenzo C, Fourrier-Reglat A, et al. Individual NSAIDs and upper gastrointestinal complications. Drug Saf. 2012;35:11127–46.
Lanas A, Wu P, Medin J, Mills EJ. Low doses of acetylsalicylic acid increase risk of gastrointestinal bleeding in a meta-analysis. Clin Gastroenterol Hepatol. 2011;9:762–8.
Tramèr MR, Moore AR, Reynolds JM, McQuay HJ. Quantitative estimation of rare adverse events which follow a biological progression: a new model applied to chronic NSAID use. Pain. 2000;85:169–82.
Yusuf S, Zhao F, Metha SR, et al. Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. N Engl J Med. 2001;345:494–502.
Ma L, Elliott SN, Cirino G, Buret A, Ignarro LJ, Wallace JL. Platelets modulate gastric ulcer healing: role of endostatin and vascular endothelial growth factor release. Proc Natl Acad Sci U S A. 2001;98:6470–5.
Grove EL, Würtz M, Schwarz P, Jørgensen NR, Vestergaard P. Gastrointestinal events with clopidogrel: a nationwide population-based cohort study. J Gen Intern Med. 2013;28:216–22.
Gurwitz JH, Goldberg RJ, Holden A, Knapic N, Ansell J. Age-related risks of long term oral anticoagulant therapy. Arch Intern Med. 1988;148:1733–6.
Fitzmaurice DA, Blann AD, Lip GYH. Bleeding risks of antithrombotic therapy. BMJ. 2002;325:828–31.
Gallagher AM, van Staa TP, Murray-Thomas T, et al. Population-based cohort study of warfarin-treated patients with atrial fibrillation: incidence of cardiovascular and bleeding outcomes. BMJ Open. 2014;4:e003839. https://doi.org/10.1136/bmjopen-2013-003839.
Taylor FC, Cohen H, Ebrahim S. Systematic review of long term anticoagulation or antiplatelet treatment in patients with non-rheumatic atrial fibrillation. BMJ. 2001;322:321–6.
Ruff CT, Guigliano RP, Braunwald E, Hoffman EB, Deenadayalu N, et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet. 2014;383:955–62.
Zhu J, Alexander GC, Nazarian S, Segal JB, Wu AW. Trends and variation in oral anticoagulant choice in patients with atrial fibrillation. Pharmacotherapy. 2018;38:907–20. https://doi.org/10.1002/phar.2158.
Abraham NS, Noseworthy PA, Yao X, Sangaralingham LR, Shah ND. Gastrointestinal safety of direct oral anticoagulants: a large population-based study. Gastroenterology. 2016;152:1014–22.
Vinogradova Y, Coupland C, Hill T, Hippisley-Cox J. Risks and benefits of direct oral anticoagulants versus warfarin in a real world setting: cohort study in primary care. BMJ. 2018;362:k2505.
Eikelboom JW, Connolly SJ, Bosch J, Dagenais GR, Hart RG, Shestakovska O, et al. Rivaroxaban with or without aspirin in stable cardiovascular disease. N Engl J Med. 2017;377:1319–30.
Sørensen R, Hansen ML, Abildstrom SZ, Hvelplund A, Andersson C, Jørgensen C, et al. Risk of bleeding in patients with acute myocardial infarction treated with different combinations of aspirin, clopidogrel, and vitamin K antagonists in Denmark: a retrospective analysis of nationwide registry data. Lancet. 2009;374:1967–74.
Ramamoorthy S, Cidlowski JA. Corticosteroid-mechanisms of action in health and disease. Rheum Dis Clin N Am. 2017;42:15–31.
Martinek J, Hlavova K, Zavada F, et al. “A surviving myth”—corticosteroids are still considered ulcerogenic by a majority of physicians. Scand J Gastroenterol. 2010;45:1156–61.
Narum S, Westergren T, Klemp M. Corticosteroids and risk of gastrointestinal bleeding: a systematic review and meta-analysis. BMJ Open. 2014;4:e004587. https://doi.org/10.1136/bmjopen-2013-004587.
Hemels ME, Koren G, Einarson TR. Increased use of antidepressants in Canada: 1981–2000. Ann Pharmacother. 2002;36:1375–9.
Ford AC, Lacy BE, Harris LA, Quigley EMM, Moayyedi P. Effect of antidepressants and psychological therapies in irritable bowel syndrome: an updated systematic review and meta-analysis. Am J Gastroenterology. 2019;114:21–39.
MacGillivray S, Arroll B, Hatcher S, Ogston S, Reid I, Sullivan F, et al. Efficacy and tolerability of selective serotonin reuptake inhibitors compared with tricyclic antidepressants in depression treated in primary care: systematic review and meta-analysis. BMJ. 2003;326:1014. https://doi.org/10.1136/bmj.326.7397.1014.
Serebruany VL. Selective serotonin reuptake inhibitors and increased bleeding risk: are we missing something? Am J Med. 2006;119:113–6.
Andrade C, Sandarsh S, Chethan KB, et al. Serotonin reuptake inhibitor antidepressants and abnormal bleeding: a review for clinicians and a reconsideration of mechanisms. J Clin Psychiatry. 2010;71:1565–75.
Abdel Salam OM. Fluoxetine and sertraline stimulate gastric acid secretion via a vagal pathway in anaesthetised rats. Pharmacol Res. 2004;50:309–16.
de Abajo FJ, Rodriguez LA, Montero D. Association between selective serotonin reuptake inhibitors and upper gastrointestinal bleeding: population based case-control study. BMJ. 1999;319:1106–9.
Dalton SO, Johansen C, Mellemkjaer L, et al. Use of selective serotonin reuptake inhibitors and risk of upper gastrointestinal tract bleeding: a population-based cohort study. Arch Int Med. 2003;163:59–64.
Anglin R, Yuan YH, Moayyedi P, Tse F, Armstrong D, Leontiadis GI. Risk of upper gastrointestinal bleeding with selective serotonin reuptake inhibitors with or without concurrent nonsteroidal anti-inflammatory use: a systematic review and meta-analysis. Am J Gastroenterol. 2014;109:811–9.
Guo C-G, Cheung KS, Zhang F, Chan EW, Chen L, Wong ICK, et al. Risks of hospitalization for upper gastrointestinal bleeding in users of selective serotonin reuptake inhibitors after Helicobacter pylori eradication therapy: a propensity score matching analysis. Aliment Pharmacol Ther. 2019;50:1001–8.
Hooi JKY, Lai WY, Ng WK, Suen MMY, Underwood FE, Tanyingoh D, et al. Global prevalence of Helicobacter pylori infection: systematic review and meta-analysis. Gastroenterology. 2017;153:420–9.
Crowe SE. Helicobacter pylori infection. NEJM. 2019;380:1158–65.
Huang J-Q, Sridhar S, Hunt RH. Role of Helicobacter pylori infection and non-steroidal anti-inflammatory drugs in peptic-ulcer disease: a meta-analysis. Lancet. 2002;359:14–22.
Ng JC, Yeomans ND. Helicobacter pylori infection and the risk of upper gastrointestinal bleeding in low dose aspirin users: systematic review and meta-analysis. Med J Austr. 2018;209:306–11.
Krag M, Perner A, Wetterslev J, et al. Prevalence and outcome of gastrointestinal bleeding and use of acid suppressants in acutely ill adult intensive care patients. Intensive Care Med. 2015;41:833–45.
Cook DJ, Griffith LE, Walter SD, Guyatt GH, Meade MO, Heyland DK, et al. The attributable mortality and length of intensive care unit stay of clinically important gastrointestinal bleeding in critically ill patients. Crit Care. 2001;5:368–75.
Rockall TA, Logan RF, Devlin HB, Northfield TC. Risk assessment after acute upper gastrointestinal haemorrhage. Gut. 1996;38:316–21.
Blatchford O, Murray WR, Blatchford M. A risk score to predict need for treatment for upper-gastrointestinal haemorrhage. Lancet. 2000;356:1318–21.
Leontiadis GI, Molloy-Bland M, Moayyedi P, Howden CW. Effect of comorbidity on mortality in patients with peptic ulcer bleeding: systematic review and meta-analysis. Am J Gastroenterol. 2013;108:331–45.
Ford AC, Gurusamy KS, Delaney B, Forman D, Moayyedi P. Eradication therapy for peptic ulcer disease in Helicobacter pylori-positive people. Cochrane Database Syst Rev. 2016;(4):Art. No.: CD003840. https://doi.org/10.1002/14651858.CD003840.pub5.
Gabriel SE, Jaakkimainen L, Bombardier C. Risk for serious gastrointestinal complications related to use of nonsteroidal anti-inflammatory drugs. A meta-analysis. Ann Intern Med. 1991;115:787–96.
Silverstein FE, Graham DY, Senior JR, et al. Misoprostol reduces serious gastrointestinal complications in patients with rheumatoid arthritis receiving nonsteroidal anti-inflammatory drugs. Ann Intern Med. 1995;123:241–9.
Lee S-J, Shin D-H, Hwang H-J, Kim JY, Pak HN, Lee MH, et al. Bleeding risk and major adverse events in patients with previous ulcer on oral anticoagulation therapy. Am J Cardiol. 2012;110:373–7.
Gisbert JP, Pajares JM. Systematic review and meta-analysis: is 1-week proton pump inhibitor-based triple therapy sufficient to heal peptic ulcer? Aliment Pharmacol Ther. 2005;21:795–804.
Gisbert JP, Khorrami S, Carballo F, Calvet X, Gené E, Dominguez-Muñoz E. Helicobacter pylori eradication therapy vs. antisecretory non-eradication therapy (with or without long-term maintenance antisecretory therapy) for the prevention of recurrent bleeding from peptic ulcer. Cochrane Database of Syst Rev. 2004;(2):Art. No.: CD004062. https://doi.org/10.1002/14651858.CD004062.pub2.
Moayyedi P, Feltbower R, Brown J, Mason S, Mason J, Nathan J, et al. Effect of population screening and treatment for Helicobacter pylori on dyspepsia and quality of life in the community: a randomised controlled trial. Lancet. 2000;355:1665–9.
Lane JA, Murray LJ, Noble S, Egger M, Harvey IM, Donovan JL, et al. Impact of Helicobacter pylori eradication on dyspepsia, health resource use, and quality of life in the Bristol helicobacter project: randomised controlled trial. BMJ. 2006;332:199–204. https://doi.org/10.1136/bmj.38702.662546.55.
IARC Helicobacter pylori Working Group. Helicobacter pylori eradication as a strategy for preventing gastric cancer. IARC Working Group Reports 8.
Fock KM, Katelaris P, Sugano K, Ang TL, Hunt RH, Talley NJ, et al. Second Asian-Pacific Consensus Guidelines for Helicobacter pylori eradication. J Gastroenterol Hepatol. 2009;24:1587–600.
Ford AC, Yuan Y, Forman D, Hunt R, Moayyedi P. Helicobacter pylori eradication for the prevention of gastric neoplasia. Cochrane Database Syst Rev. 2020;(7):Art. No.: CD005583. https://doi.org/10.1002/14651858.CD005583.pub3.
Ford AC, Yuan Y, Moayyedi P. Helicobacter pylori eradication therapy to prevent gastric cancer: systematic review and meta-analysis. Gut 2020;69: 2113–21. https://doi.org/10.1136/gutjnl-2020-320839.
GBD 2017 Stomach Cancer Collaborators. The global, regional, and national burden of stomach cancer in 195 countries, 1990–2017: a systematic analysis for the Global Burden of Disease study 2017. Lancet Gastroenterol Hepatol. 2020;5:42–54.
Ford AC, Forman D, Bailey AG, Axon ATR, Moayyedi P. A community screening program for Helicobacter pylori saves money: 10-year follow-up of a randomised controlled trial. Gastroenterology. 2005;129:1910–7.
Mason J, Axon ATR, Forman D, Duffett S, Drummond M, Crocombe W, et al. The cost-effectiveness of population Helicobacter pylori screening and treatment: a Markov model using economic data from a randomised controlled trial. Aliment Pharmacol Ther. 2002;16:559–68.
Harvey RF, Lane JA, Nair P, Egger M, Harvey I, Donovan J, et al. Clinical trial: prolonged beneficial effect of Helicobacter pylori eradication on dyspepsia consultations - the Bristol helicobacter project. Aliment Pharmacol Ther. 2010;32:394–400.
Chey WD, Leontiadis GI, Howden CW, Moss SF. ACG clinical guideline: treatment of Helicobacter pylori infection. Am J Gastroenterol. 2017;112:212–39. https://doi.org/10.1038/ajg.2016.563.
Chan FK, Ching JY, Suen BY, et al. Effects of Helicobacter pylori infection on long-term risk of peptic ulcer bleeding in low-dose aspirin users. Gastroenterology. 2013;144:528–35.
Vergara M, Catalan M, Gisbert JP, Calvet X. Meta-analysis: role of Helicobacter pylori eradication in the prevention of peptic ulcer in NSAID users. Aliment Pharmacol Ther. 2005;21:1411–8.
Leontiadis GI, Sreedharan A, Dorward S, et al. Systematic reviews of the clinical effectiveness and cost-effectiveness of proton pump inhibitors in acute upper gastrointestinal bleeding. Health Technol Assess. 2007;11:iii-iv 1–164.
Lanza FL, Chan FK, Quigley EM. Guidelines for prevention of NSAID-related ulcer complications. Am J Gastroenterol. 2009;104:728–38.
Laine L, Takeuchi K, Tarnawski A. Gastric mucosal defense and cytoprotection: bench to bedside. Gastroenterology. 2008;135:41–60.
Scally B, Emberson JR, Spata E, Reith C, Davies K, Halls H, et al. Effects of gastroprotectant drugs for the prevention and treatment of peptic ulcer disease and its complications: meta-analysis of randomised trials. Lancet Gastroenterol Hepatol. 2018;3:231–41.
Rostom A, Dube C, Wells GA, Tugwell P, Welch V, Jolicoeur E, et al. Prevention of NSAID-induced gastroduodenal ulcers. Cochrane Database Syst Rev. 2002;(4):Art. No.: CD002296. https://doi.org/10.1002/14651858.CD002296.
Causada-Calo N, Germini F, Yuan Y, Eikelboom JW, Moayyedi P. Proton-pump inhibitors for the prevention of upper gastrointestinal bleeding in adults receiving antithrombotic therapy. Cochrane Database of Syst Rev. 2019;(8):Art. No.: CD013415. https://doi.org/10.1002/14651858.CD013415.
Causada-Calo N, Germini F, Yuan Y, Eikelboom JW, Moayyedi P. Clopidogrel-based antithrombotic therapy for cardiovascular prevention: a systematic review and meta-analysis of randomized controlled trials. Gastroenterology. 2019;156(supplement 1):S97.
•• Moayyedi P, Eikelboom JW, Bosch J, et al. Safety of proton pump inhibitors based on a large, multi-year, randomized trial of patients receiving rivaroxaban or aspirin. Gastroenterology. 2019;157:682–91 Largest RCT in gastroenterology evaluating a pharmacological intervention and the first to evaluate PPI in patients taking anticoagulation. This trial suggested that PPI therapy reduced the risk of peptic ulcer and peptic ulcer bleeding, but the event rate was too low for this to be cost-effective in all patients taking anticoagulation.
Alhazzani W, Alenezi F, Jaeschke RZ, Moayyedi P, Cook DJ. Proton pump inhibitors versus histamine 2 recpetor antagonists for stress ulcer prophylaxis in critically ill patients: a systematic review and meta-analysis. Crit Care Med. 2013;41:693–705.
Alshamsi F, Belley-Cote E, Cook D, Almenawer SA, Alqahtani Z, Perri D, et al. Efficacy and safety of proton pump inhibitors for stress ulcer prophylaxis in critically ill patients: a systematic review and meta-analysis of randomized trials. Crit Care. 2016;20:120. https://doi.org/10.1186/s13054-016-1305-6 PMID: 27142116; PMCID: PMC4855320.
•• Wang Y, Ye Z, Ge L, et al. Efficacy and safety of gastrointestinal bleeding prophylaxis in critically ill patients: systematic review and network meta-analysis. BMJ. 2020;368:l6744. https://doi.org/10.1136/bmj.l6744Comprehensive network meta-analysis of all treatment options to prevent stress ulcer bleeding in intensive care patients. Acid suppressive therapy was effective but probably not beneficial in low risk patients.
Moayyedi P, Santana J, Khan M, Preston C, Donnellan C. Medical treatments in the short term management of reflux oesophagitis. Cochrane Database Syst Rev. 2007;(2):Art. No.: CD003244. https://doi.org/10.1002/14651858.CD003244.pub2.
Vaezi M, Yang Y-X, Howden CW. Complications of proton pump inhibitor therapy. Gastroenterology. 2017;153:35–48.
Laheij RJ, Sturkenboom MC, Hassing RJ, et al. Risk of community-acquired pneumonia and use of gastric acid suppressive drugs. JAMA. 2004;292:1955–60.
Yang YX, Lewis JD, Epstein S, Metz DC. Long-term proton pump inhibitor therapy and risk of hip fracture. JAMA. 2006;296:2947–53.
Neal KR, Scott HM, Slack RCB, Logan RF. Omeprazole as a risk factor for campylobacter gastroenteritis: case-control study. BMJ. 1996;312:414–5.
Charlot M, Grove EL, Hansen PR, Olesen JB, Ahlehoff O, Selmer C, et al. Proton pump inhibitor use and risk of adverse cardiovascular events in aspirin treated patient with first time myocardial infarction: a nationwide propensity score matched analysis. BMJ. 2011;342:d2690.
Lazarus B, Chen Y, Wilson FP, Sang Y, Chang AR, Coresh J, et al. Proton pump inhibitor use and risk of chronic kidney disease. JAMA Intern Med. 2016;176:238–46.
Gomm W, von Holt K, Thome F, Broich K, Maier W, et al. Association of proton pump inhibitors with risk of dementia: a pharmacoepidemiological claims data analysis. JAMA Neurol. 2016;73:410–6.
Cheung KS, Chan EW, Wong AYS, Chen L, Wong ICK, Leung WK. Long-term proton pump inhibitors and risk of gastric cancer development after treatment for helicobacter pylori: a population-based study. Gut. 2018;67:28–35.
Xie Y, Bowe B, Li T, Xian H, Yan Y, Al-Aly Z. Risk of death among users of proton pump inhibitors: a longitudinal observational cohort study of United States veterans. BMJ Open. 2017;7(6):e015735.
Simonov M, Abel EE, Skanderson M, et al. Use of proton pump inhibitors increases risk of incident kidney stones. Clin Gastroenterol Hepatol. 2020. https://doi.org/10.1016/j.cgh.2020.02.053 In press.
Moayyedi P. Leaving no stone unturned in the search for adverse events associated with the use of proton pump inhibitors. Clin Gastroenterol Hepatol. 2020. https://doi.org/10.1016/j.cgh.2020.04.053 in press.
Almario CV, Chey WD, Spiegel BMR. Increased risk of COVID-19 among users of proton pump inhibitors. Am J Gastroenterol. 2020;115:1707–15.
Moayyedi P, Leontiadis GI. The risks of PPI therapy. Nature Reviews of Gastroenterology & Hepatology. 2012;9:132–9.
• Moayyedi P, Eikelboom JW, Bosch J, et al. Safety of proton pump inhibitors based on a large, multi-year, randomized trial of patients receiving rivaroxaban or aspirin. Gastroenterology. 2019;157:682–91 This trial evaluated the safety of PPIs with over 53,000 patients years of follow-up. There was no evidence of harm of PPIs apart from risk of enteric infections and the data suggested that the various harms of PPI described in observational studies are likely to be overestimated.
Attwood SE, Ell C, Galmiche JP, Fiocca R, Hatlebakk JG, Hasselgren B, et al. Long-term safety of proton pump inhibitor therapy assessed under controlled, randomised clinical trial conditions: data from the SOPRAN and LOTUS studies. Aliment Pharmacol Ther. 2015;41:1162–74.
Jankowski JA, de Caestecker J, Love SB, et al. Esomeprazole and aspirin in Barrett’s oesophagus (AspECT): a randomised factorial trial. Lancet. 2018;392:400–8.
• Ho PM, Maddox TM, Wang L, et al. Risk of adverse outcomes associated with concomitant use of clopidogrel and proton pump inhibitors following acute coronary syndrome. JAMA. 2009;301:937–44 The first randomized trial evaluating PPI and aspirin to prevent progression of Barrett’s esophagus to neoplasia. If this trial started today there would be objection to such high doses of PPI being used for an average of 9 years, but mortality was reduced in the twice daily PPI group. The GI bleeding rate was very low in this trial giving indirect evidence to the benefit of this approach.
Garcia-Rayado G, Navarro M, Lanas A. NSAID induced gastrointestinal damage and designing GI-sparing NSAIDs. Expert Rev Clin Pharmacol. 2018;11:1031–43.
Deeks JJ, Smith LA, Bradley MD. Efficacy, tolerability, and upper gastrointestinal safety of celecoxib for treatment of osteoarthritis and rheumatoid arthritis: systematic review of randomised controlled trials. BMJ. 2002;325:619–23.
Rostom A, Muir K, Dubé C, Jolicoeur E, Boucher M, Joyce J, et al. Gastrointestinal safety of cyclooxygenase-2 inhibitors: a Cochrane collaboration systematic review. Clin Gastroenterol Hepatol. 2007;5:818–28.
Bresalier RS, Sandler RS, Quan H, Bolognese JA, Oxenius B, Horgan K, et al. Cardiovascular events associated with rofecoxib in a colorectal adenoma chemoprevention trial. New Engl J Med. 2005;352:1092–102.
Solomon SD, McMurray JJ, Pfeff er MA, et al. Cardiovascular risk associated with celecoxib in a clinical trial for colorectal adenoma prevention. New Engl J Med. 2005;352:1071–80.
Coxib and traditional NSAID Trialists’ (CNT) Collaboration. Vascular and upper gastrointestinal effects of non-steroidal anti-inflammatory drugs: meta-analyses of individual participant data from randomised trials. Lancet. 2013;382:769–79.
Jordan F, Quinn TJ, McGuinness B, Passmore P, Kelly JP, Tudur Smith C, et al. Aspirin and other non-steroidal anti-inflammatory drugs for the prevention of dementia. Cochrane Database Syst Rev. 2020;(4):Art. No.: CD011459. https://doi.org/10.1002/14651858.CD011459.pub2.
Raskin JB, White RH, Jackson JE, Weaver AL, Tindall EA, Lies RB, et al. Misoprostol dosage in the prevention of nonsteroidal anti-inflammatory drug-induced gastric and duodenal ulcers: a comparison of three regimens. Ann Intern Med. 1995;123:344–50.
Taha AS, McCloskey C, McSkimming P, McConnachie A. Misoprostol for small bowel ulcers in patients with obscure bleeding taking aspirin and non-steroidal anti-inflammatory drugs (MASTERS): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Gastroenterol Hepatol. 2018;3:469–76.
Sheridan S, Pignone M, Mulrow C. Framingham-based tools to calculate the global risk of coronary heart disease. J Gen Intern Med. 2003;18:1039–52.
Fallone CA, Gisbert JP, Chiba N, van Zanten SV, Fischbach L, et al. The Toronto helicobacter pylori consensus in context reply. Gastroenterology. 2017;152:303–4.
Granholm A, Zeng L, Dionne JC, et al. Predictors of gastrointestinal bleeding in adult ICU patients: a systematic review and meta-analysis. Intensive Care Med. 2019;45:1347–59.
Bo M, Gibello M, Brunetti E, Boietti E, Sappa M, Falcone Y, et al. Prevalence and predictors of inappropriate prescribing according to the screening tool of older people’s prescriptions and screening tool to alert to right treatment version 2 criteria in older patients discharged from geriatric and internal medicine wards: a prospective observational multicenter study. Geriatr Gerontol Int. 2019;19:5–11.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Takeshi Kanno declares that he has no conflict of interest. Paul Moayyedi declares that he has no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kanno, T., Moayyedi, P. Who Needs Gastroprotection in 2020?. Curr Treat Options Gastro 18, 557–573 (2020). https://doi.org/10.1007/s11938-020-00316-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11938-020-00316-9