Abstract
Colorectal cancer (CRC) screening rates are low among Latinos. To identify factors associated with CRC screening, we conducted a telephone survey of Latino primary care patients aged 50–79 years. Among 1,013 participants, 38% were up-to-date (UTD) with fecal occult blood test (FOBT); 66% were UTD with any CRC screening (FOBT, sigmoidoscopy, or colonoscopy). Individuals less than 65, females, those less acculturated, and patients of female physicians were more likely to be UTD with FOBT. CRC screening among Latinos is low. Younger patients, women, and patients of female physicians receive more screening.
Similar content being viewed by others
Background
Colorectal cancer (CRC) is the second leading cause of cancer death. Screening for CRC results in earlier detection and improved survival. The US Preventive Services Task Force recommends screening for CRC for all persons over 50 but recommends no preferred screening strategy [1]. The American Cancer Society, the US Multi-society Task Force on Colorectal Cancer, and the American College of Radiology have recently published new joint guidelines that encourage clinicians to make patients aware of the full range of screening options [2]. However, all screening tests may not be available in all settings, especially in resource poor settings.
Despite clear benefits, screening rates are still low. In 2004, only 18.7% of US adults aged 50 and over had undergone fecal occult blood test (FOBT) within the preceding year, only 50.6% of eligible participants had undergone sigmoidoscopy/colonoscopy (SIG/COL) in the preceding 10 years, and only 57% of US adults over age 50 have been recently screened with FOBT or SIG/COL [3].
CRC screening rates are lower in Latinos than in non-Latino whites. In 2003, only 11.9% of Latinos reported completing an FOBT in the past year, compared with 16.3% for non-Latino whites; only 25.1% of Latinos had a lower SIG/COL rate in the past 5 years, compared with 37.5% among non-Latino whites [4]. In a recent survey of community-dwelling Latinos, Vietnamese, and whites, we found that Latinos were less likely to be up-to-date with CRC screening than whites [5]. Among non-English speakers, rates were particularly low. For example, 66% of English speakers compared with 15% of Spanish speakers reported receiving SIG in the past 5 years (p < 0.01). These disparities parallel those for mammography in the early years of breast cancer screening guidelines [6]. Though Latinos tend to receive less breast and cervical cancer screening compared with non-Latino whites (66% vs 71% and 75% vs 80% for breast and cervical cancer, respectively), the gap in screening for these cancers has narrowed over the last several years, whereas the gap in screening for CRC has largely remained unchanged [7].
Many factors influence whether or not an individual receives CRC screening. A previous telephone survey of Latinos conducted in Santa Clara, California, revealed that embarrassment about the screening tests was a significant reason to forego screening, a factor that was not accorded nearly as much importance by whites [5]. The biggest factor influencing screening was physician recommendation [5]. Lack of knowledge and fatalistic attitudes about screening and cancer have also been identified among Latinos [8]. Other barriers for underserved populations include language and acculturation [9-11]. While these studies have typically included community samples in which individuals may not have access to care, less is known about barriers to CRC screening among individuals who have a source of primary care. In the primary care setting, both patient and physician-mediated factors can affect rates of CRC screening [12].
In this report, we identify and analyze patient and physician factors associated with receipt of CRC screening among Latinos seen in primary care clinics in a county medical system.
Methods
Setting
As part of an intervention to increase rates of CRC screening in Latino and Vietnamese patients at Santa Clara Valley Medical Center (SCVMC), a public hospital owned and operated by the county, a baseline telephone survey was conducted between September 2005 and May 2006. Due to limited endoscopy capacity, the primary screening option offered at SCVMC is FOBT. Colonoscopies are performed in individuals who have a family history, are symptomatic, or for the evaluation of a positive FOBT test, but are not otherwise offered as primary screening.
Participants
Participants were Latino men and women who are patients at five SCVMC primary care satellite sites. All primary care physicians seeing patients at the medical center were invited to participate and asked for permission to contact their eligible Latino patients aged 50–79. Exclusion criteria included dementia or any condition (e.g., terminal illness) for which the physician deemed the patient ineligible for screening. After the physician gave permission, eligible patients received a letter describing the study, enclosing a refusal postcard. Individuals who did not return the postcard received a phone call asking them to participate. Those who participated in the telephone interview received $15.00 cash after survey completion.
Data Collection Instrument
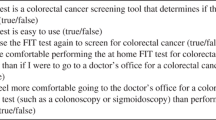
The telephone interview was developed based on our prior survey of barriers to CRC screening in Vietnamese, Latinos, and whites [5]. The survey was developed in English, translated into Spanish, and back-translated into English to ensure lexical equivalency; it was pilot tested and revised. This methodology ensured that the source language did not become the dominant language [13].
Items included demographics, acculturation, perceived health status, previous CRC screening behaviors, intention to be screened, beliefs, knowledge, and perceived barriers and facilitators to screening. We asked five knowledge questions and derived a summary knowledge score, which was calculated as the number of the five knowledge items answered correctly. We asked questions about acculturation, using a five-item scale developed by Marin and Sabogal and previously used and validated in the Latino population [14]. A high value denotes high acculturation.
The survey was administered by trained bilingual interviewers and conducted in Spanish or English, depending on the participant's choice. Institutional Review Board approval was obtained from all institutions.
Analyses
Data were analyzed using SAS [15]. The primary analyses were designed to examine the association of the outcome variables (up-to-date with FOBT, SIG/COL, or any CRC screening) with sociodemographics, knowledge, and provider characteristics. Descriptive statistics were computed for all demographic and dependent variables, including means and standard deviations for continuous data and frequency distributions for each of the categorical variables.
Initial univariate analyses were conducted based on frequency tables of the outcomes and potential covariates; chi-square tests, student's test, and logistic regression models were used to gauge the degree of association. Results were used to make informed decisions about which variables to include in the final models. Given that both patients and physicians are instrumental in determining whether screening is completed, we included both patient and physician factors.
In the multivariate logistic regression model, we explored which patient and physician factors were independently associated with being up-to-date with screening. We included six sociodemographic factors (age, gender, marital status, education, employment, and acculturation) and factors that we hypothesized would be related to self-rated health, perceived risk of cancer, a measure of CRC awareness, and a summary CRC knowledge score. We also included physician factors of gender, gender concordance, ethnicity concordance, and language concordance.
In our prior work, the biggest predictor of receipt of CRC screening was physician recommendation. When this variable was excluded, several additional variables became significant [5]. Consequently, we present a model that does not include physician recommendation for the additional reason that it is not possible to obtain screening without physician recommendation. The estimates of these parameters of multivariate logistic regression models were computed in a stepwise manner by entering or removing variables one variable at a time from the potential predictors. The entry criterion of p = 0.30 and the removal criteria of p = 0.35 was set for entering and removing variables in the stepwise models. All predictors were presented in the final parsimonious model; those variables showing a significant effect (p < 0.05) are marked with an asterisk.
Results
Provider Characteristics
Of 49 physicians asked to participate, 44 (90%) agreed. Among participants, 23 (56%) were female, half (51%) were Caucasian, 10% were Latino, and the remainder were of other ethnicities. About half (51%) spoke Spanish. On average, physicians were in clinical practice about 6.5 half-day sessions per week, and 42 (95%) were US graduates.
Patient Characteristics
Call attempts were made to 2,018 of 2,147 eligible individuals who had not returned refusals (Table 1). A total of 1,013 completed the survey (response rate of 47%).
The average age was 60.4 years, about 75% were female, and less than half were married or living with a partner. The majority (80%) was born outside the USA and had lived in the USA for an average of 23 years. Less than 25% were employed, one third were homemakers, and the remainder were retired or not working. Among those who reported annual household income (70%), over half had incomes of <$20,000/year. Over two thirds reported having six or fewer years of formal education. The majority (83%) completed the interview in Spanish. To assess acculturation, we used a previously developed acculturation scale, where a score of <2.99 is “low acculturated” and a score of 3.0 or greater is “high acculturated”; 81% of Latinos were “low acculturated” [14]. On a self-rated scale of excellent, good, fair, and poor, about half rated their health as “fair” (55%), and only 17% thought their risk of CRC was higher than others their age.
Most had heard of CRC (79%), although less than half had heard of a polyp, FOBT, SIG, or COL (30%, 49%, 36%, and 35%, respectively). Thirty-eight percent had an FOBT in the last year, 13% reported a SIG in the last 5 years, and 17% had a COL in the last 10 years. Overall, just over half were up-to-date with any CRC screening (FOBT in the past year, SIG in the past 5 years, or COL in the past 10 years; 51%).
CRC knowledge was measured by five items. About 40% thought that that if they ate a healthy diet, they did not need screening; and approximately two thirds (63%) agreed that there were “too many twists and turns in the intestines to find CRC when it was small.” About one third thought that if a doctor examined their rectum with his/her finger, that they did not need another test. Over two thirds agreed that “if a CRC test comes out normal then you do not need any more tests.” Over half (58%) thought that they “did not need a CRC test until they had stomach problems.” The average summary knowledge score was three correct.
Over half (60%) stated that a physician had recommended FOBT, but less than a quarter (23%) reported ever requesting an FOBT.
Predictors of Up-to-date Screening
All outcomes (FOBT in the past year, SIG in the past 5 years, or COL in the past 10 years, and any CRC screening) are reported, with particular focus on the main outcome for the intervention, FOBT in the past year and any CRC screening. Since results were similar for both SIG in the past 5 years and COL in the past 10 years, we present these as a combined outcome—either SIG in the past 5 years or COL in the past 10 years.
Multivariate Analyses
In the multivariate model, patient factors significantly associated with being up-to-date with FOBT screening were aged <65 (odds ratio (OR) 1.40, 95% confidence interval (CI) 1.03–1.90), being female (OR 1.89, 95% CI 1.17–3.05), low level of acculturation (OR 0.46, 95% CI 0.30–0.70), and having a female physician (OR 2.17, 95% CI 1.58–3.00; Table 2). Individuals who had language concordance with their physicians were less likely to receive FOBT (OR 0.55, (95% CI 0.40, 0.76). The only factor associated with being up-to-date with SIG/COL was having 13 years or more of education compared with 6 or less (OR 2.57, 95% CI 1.54–4.32). Factors independently associated with being up-to-date were being female (OR 1.68, 95% CI 1.06–2.66), having 13 years of education compared with 6 or less (OR 2.33, 95% CI 1.39–3.91), and being of low acculturation (OR 0.62, 95% CI 0.42–0.92). Individuals who had a female physician were more likely to receive any CRC screening than those who did not (OR 1.80, 95% 1.32–2.46).
Discussion
Even in a primary care clinic population, CRC screening rates are still sub-optimal; only about half of respondents were up-to-date, which is comparable to national rates from a community-based sample [3]. Even in this population where all individuals have access to care, many are not receiving CRC screening.
Individuals younger than 65 were more likely to be up-to-date. This is in contrast to a prior study in a multi-ethnic population where individuals aged 50–64 were less likely to be screened than older individuals [16]. Latinos with more education were more likely to be up-to-date with endoscopic or any CRC screening, which comports with findings of prior studies [17].
In our study, Latino women were more likely to be up-to-date with screening than were men, although in the California Health Interview survey, a community-based survey of a diverse population of participants, men were more likely to be tested than women [17]. It may be that women who are seen in primary care clinic settings are more used to undergoing regular screening tests such as mammography and Pap smears and hence also receive FOBT.
Individuals who were less acculturated were more likely to be up-to-date with FOBT or any CRC screening. It is possible that those who are more acculturated may be opting more for endoscopic screening, which may reflect the public perspective that has been widespread in the media that COL is a “better” test. A prior study showed that low acculturation was associated with less endoscopic screening, but acculturation was not associated with FOBT screening [18]. Alternatively, it is possible that those who are less acculturated are less likely to question their physician and have testing if it is recommended.
Although there was an association of two knowledge questions with CRC screening in univariate models, the overall knowledge score was only associated with endoscopic screening.
Physician factors affected the likelihood of receiving CRC screening. Individuals who had female physicians were more likely to receive screening than those with male physicians. Prior studies have shown that women physicians do more screening for female cancers such as breast and cervix [19-22] as well as more counseling and immunization for and about gender-neutral recommendations. This suggests that women physicians may have an overall greater prevention orientation, rather than the screening being related to gender concordance between patient and physician [23]. Although previous studies have suggested that physician–patient communication may be enhanced and or that physicians' decision making styles may be more participatory when physicians and patients belong to the same race [24, 25], this did not translate into an increase in screening in our study.
Surprisingly, language concordance was not associated with increased screening; in fact, patients whose physicians spoke Spanish were less likely to receive FOBT. In a prior study, language concordance positively influenced agreement about exercise but negatively influenced agreement about medication use [26]. For CRC screening, it is possible that Spanish-speaking physicians would know of a possible cultural distaste for discussing these matters and they may not bring it up. Further studies on the relationship between language concordance and health outcomes are needed.
Our study had several limitations. Participants were drawn from a single geographic setting, with Latinos who were mostly Spanish speaking, and of low acculturation with little formal education, thus these results may not be representative of Latinos in different geographic settings or those who are more acculturated or more highly educated. Second, those who participated in the survey are probably those with more interest in screening and are thus more likely to be screened. It is likely that the overall rate of screening among all clinic patients is lower than that reported here. In addition, SCVMC is a site that already strives to provide culturally sensitive care; they provide many educational materials in Spanish and have a readily accessible interpreter service. Finally, causality cannot be inferred from a cross-sectional survey.
Despite the limitations, this study provides important information about the contribution of patient and physician factors to receipt of CRC screening in Latinos. Younger individuals, women, and those who were more educated are more likely to be up-to-date with screening. Even for this gender-neutral cancer, patients of female physicians receive more screening. Although younger individuals may be more likely to be up-to-date because of increased awareness and knowledge, because the risk of CRC increases with age, it is particularly important to ensure that older individuals receive screening. Future efforts should target older Latinos, males, and those who are less educated to ensure that all receive appropriate screening. Future research should also address ways in which all physicians, regardless of gender, ethnicity, or language concordance with their patients, can encourage Latino patients to undergo recommended CRC screening.
References
United States Preventive Services Task Force (2002) Screening for colorectal cancer: recommendation and rationale. Ann Intern Med 137(2):129–131
Levin B, Lieberman DA, McFarland B et al (2008) Screening and surveillance for the early detection of colorectal cancer and Adenomatous Polyps, 2008: a joint guideline from the American Cancer Society, the US multi-society task force on colorectal cancer, and the American College of radiology. CA Cancer J Clin 58(3):130–160
Morbidity and Mortality Weekly Report (2006) Increased use of colorectal cancer tests—United States, 2002 and 2004. MMWR 55(11):308–311
American Cancer Society (2006) Cancer prevention and early detection facts and figures. American Cancer Society, Atlanta, pp 1–60
Walsh J, Kaplan C, Nguyen B, Gildengorin G, McPhee S, Perez-Stable E (2004) Barriers to colorectal cancer screening in Latino and Vietnamese Americans. J Gen Intern Med 19:156–166
Jemal A, Clegg LX, Ward E et al (2004) Annual report to the nation on the status of cancer, 1975-2001, with a special feature regarding survival. Cancer 101(1):3–27
American Cancer Society (2006–2008) Cancer facts & figures for Hispanics/Latinos. American Cancer Society, Atlanta
Salazar R, Walsh J, Gildengorin G, Perez-Stable E (2003) Impacts of beliefs on colorectal cancer screening in Latinos. Paper presented at Society of General Internal Medicine 26th annual meeting
Beach M, Flood A, Robinson C et al (2007) Can language-concordant prevention care managers improve cancer screening rates? Cancer Epidemiol Biomark Prev 16:2058–2064
Jo A, Maxwell A, Wong W, Bastani R (2008) Colorectal cancer screening among underserved Korean Americans in Los Angeles County. J Immigr Minor Health 10(2):119–126
Tang TS, Solomon LJ, McCracken LM (2001) Barriers to fecal occult blood testing and sigmoidoscopy among older Chinese-American women. Cancer Pract 9(6):277–282
Walsh J, McPhee S (1992) A systems model of clinical preventive care: an analysis of factors influencing patient and physician. Health Educ Q 19(2):157–175
Pasick R, D'Onofrio C, Otero-Sabogal R (1996) Similarities and differences across cultures: questions to inform a third generation for health promotion research. Health Educ Q 23(S):s142–s161
Marin G, Sabogal F (1987) Development of a short acculturation scale for Hispanics. Hisp J Behav Sci 9:183–205
SAS 9.1.3. http://www.sas.com/index.html
Shokar NK, Carlson CA, Weller SC (2007) Prevalence of colorectal cancer testing and screening in a multiethnic primary care population. J Community Health 32(5):311–323
Etzioni DA, Ponce NA, Babey SH et al (2004) A population-based study of colorectal cancer test use: results from the 2001 California Health Interview Survey. Cancer 101(11):2523–2532
Shah M, Zhu K, Potter J (2006) Hispanic acculturation and utilization of colorectal cancer screening in the United States. Cancer Detect Prev 30(3):306–312
Lurie N, Slater J, McGovern P, Ekstrum J, Quam L, Margolis K (1993) Preventive care for women. Does the sex of the physician matter? N Engl J Med 329(7):478–482
Cassard SD, Weisman CS, Plichta SB, Johnson TL (1997) Physician gender and women's preventive services. J Women's Health 6(2):199–207
Levy S, Dowling P, Boult L, Monroe A, McQuade W (1992) The effect of physician and patient gender on preventive medicine practices in patients older than fifty. Fam Med 24(1):58–61
Franks P, Clancy CM (1993) Physician gender bias in clinical decisionmaking: screening for cancer in primary care. Med Care 31(3):213–218
Flocke SA, Gilchrist V (2005) Physician and patient gender concordance and the delivery of comprehensive clinical preventive services. Med Care 43(5):486–492
Cooper-Patrick L, Gallo JJ, Gonzales JJ et al (1999) Race, gender, and partnership in the patient-physician relationship. JAMA 282(6):583–589
Lin EH (1983) Intraethnic characteristics and the patient-physician interaction: “cultural blind spot syndrome”. J Fam Pract 16(1):91–98
Kreuter M, Lukwago S, Bucholtz R, Clark E, Sanders-Thompson V (2003) Achieving cultural appropriateness in health promotion programs: targeted and tailored approaches. Health Educ Behav 30(2):133–146
Acknowledgements
We would like to thank Drs. Longhang Nguyen, Angela Suarez, Leslie Schmidt, Ginger Roehrig, and Kevin Nguyen for their enthusiastic participation and support in recruiting participants. We would also like to thank Mr. Lowell Huang and Ms. Vivian Quach for their support in manuscript preparation.
Funding
This project was funded by the American Cancer Society under grant number TURSG PBP–105674.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Additional information
Lamkieu Nguyen MD is deceased.
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Walsh, J.M.E., Salazar, R., Kaplan, C. et al. Healthy Colon, Healthy Life (Colon Sano, Vida Sana): Colorectal Cancer Screening Among Latinos in Santa Clara, California. J Canc Educ 25, 36–42 (2010). https://doi.org/10.1007/s13187-009-0007-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13187-009-0007-z