Abstract
Objective:
To estimate the gestational age ranges that result in optimal birth outcomes for each of four risk-defined groups.
Study Design:
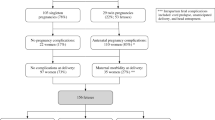
Retrospective cohort study of singleton late third-trimester deliveries at a large urban teaching hospital between July 1995 and September 2003. Low-risk, advanced maternal age, hypertensive and diabetic patients were identified and grouped. Rates, by day of gestation at delivery, of cesarean delivery, major maternal perineal trauma, low 5-min APGAR score and NICU admission were determined for each study group.
Results:
Each study group had meaningful changes in rates of obstetric outcomes as a function of gestational age at delivery and these patterns differed from group to group. A unique optimal time of delivery (OTD) was estimated for each group. The low-risk group OTD was calculated to be 37 weeks 1 day to 41 weeks 0 day; the advanced maternal age group OTD was 38 weeks 5 days to 39 weeks 6 days; the hypertension group OTD was 39 weeks 2 days to 40 weeks 1 day; and the diabetes mellitus group OTD was 40 weeks 3 days to 41 weeks 1 day.
Conclusions:
The OTD varied based on obstetrical risk. Strategies to increase the proportion of deliveries that occur within the OTD for specific risk-defined groups could theoretically improve birth outcomes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Casey BM, Lucas MJ, McIntire DD, Leveno KJ . Pregnancy outcomes in women with gestational diabetes compared with the general obstetric population. Obstet Gynecol 1997; 90: 869–873.
Remsberg KE, McKeown RE, McFarland KF, Irwin LS . Diabetes in pregnancy and cesarean delivery. Diabetes Care 1999; 22: 1561–1567.
Page EW, Christianson R . The impact of mean arterial pressure in the middle trimester upon the outcome in pregnancy. Am J Obstet Gynecol 1976; 125: 740–746.
Gofton EN, Capewell V, Natale R, Gratton RJ . Obstetrical intervention rates and maternal and neonatal outcomes of women with gestational hypertension. Am J Obstet Gynecol 2001; 185: 798–803.
Ross MG, Downey CA, Bemis-Heyes R, Nguyen M, Jacques D, Stanziano G . Prediction by maternal risk factors of neonatal intensive care admissions: evaluation of >59,000 women in national managed care programs. Am J Obstet Gynecol 1999; 181: 835–842.
Cunningham FG, MacDonald PC, Gant NF, Leveno KJ, Gilstrap LC, Hankins GDV et al. Williams Obstetrics. 20th edn. Appleton & Lange, 1997 pp 693–744; 1203–1222.
Yudkin PL, Wood L, Redman CWG . Risk of unexplained stillbirth at different gestational ages. Lancet 1987; I: 1192–1194.
Hannah ME . Postterm pregnancy: should all women have labour induced? A review of the literature. Fetal Maternal Med Rev 1993; 5: 3–17.
Clark SL, Sabey P, Jolley K . Nonstress testing with acoustic stimulation and amniotic fluid volume assessment: 5973 tests without unexpected fetal death. Am J Obstet Gynecol 1989; 160: 694–697.
Preboth A . ACOG guidelines on antepartum fetal surveillance. Am Fam Physician 2000; 62: 1184–1188.
Caughey AB, Musci TJ . Complications of term pregnancy beyond 37 weeks of gestation. Obstet Gynecol 2004; 103: 57–62.
Alexander JM, McIntire DD, Leveno KJ . Forty weeks and beyond: pregnancy outcomes by weeks of gestation. Obstet Gynecol 2000; 96: 291–293.
ACOG Committee on Practice Bulletins-Obstetrics. ACOG Practice Bulletin. Clinical management guidelines for obstetricians-gynecologists. Number 55, September 2004. Management of Postterm Pregnancy. Obstetrics & Gynecology. 104(3): 639–646, 2004 Sep.
Crowley P . Interventions for preventing or improving the outcome of delivery at or beyond term (Cochrane review) (Meta-analysis). The Cochrane Library, issue 2 Wiley: Chicester, UK, 2004.
Neilson JP . Ultrasound for fetal assessment in early pregnancy (Cochrane review) (Meta-analysis). The Cochrane Library, issue 2. Wiley: Chicester, UK, 2004.
Healthy People 2000. DHHS Publication 91-50212. US Government Printing Office: Washington, DC, 1990.
Price CJ, Kimmel CA, Tyl RW, Marr MC . The developmental toxicity of ethylene glycol in rats and mice. Toxicol Appl Pharmacol 1985; 81: 113–127.
Moerbeek M, Persma A, Slob W . A comparison of three methods for calculating confidence intervals for the benchmark dose. Risk Anal 2004; 24(1): 31–40.
Kelsall GA, Vos GH . Premature induction of labour in the treatment of haemolytic disease of the newborn. Lancet 1955; 2: 161–164.
Danforth DN . Textbook of Obstetrics and Gynecology. Harper and Row: New York, 1966, pp 301–302.
Kjos SL, Henry OA, Montoro M, Buchanan TA, Mestman JH . Insulin-requiring diabetes in pregnancy: a randomized trial of active induction of labor and expectant management. Am J Obstet Gynecol 1993; 169(3): 611–615.
Lurie S, Insler V, Hagay ZJ . Induction of labor at 38–39 weeks of gestation reduces the incidence of shoulder dystocia in gestational diabetic patients class A2. Am J Perinatol 1996; 13: 293–296.
Hannah ME, Hannah WJ, Hellmann J, Hewson S, Milner R, Willan A . Induction of labor as compared with serial antenatal monitoring in post-term pregnancy. N Engl J Med 1992; 326: 1587–1592.
Nicholson JM, Kellar LC, Cronholm PF, Macones GA . The active management of risk in pregnancy at term in an urban population: the association between a higher induction of labor rate and a lower cesarean delivery rate. Am J Obstet Gynecol 2004; 191(5): 1516–1528.
Nicholson JM, Macones GA . The active management of risk in pregnancy at term in an urban setting: the association between higher group induction of labor rates and lower group cesarean delivery rates. Am J Obstet Gynecol 2003; 189: S131.
Gafni A, Goeree R, Myhr TL, Hannah ME, Blackhouse G, Willan AR et al. Induction of labour versus expectant management for prelabour rupture of the membranes at term: an economic evaluation. Can Med Assoc J 1997; 157: 1519–1525.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nicholson, J., Kellar, L. & Kellar, G. The impact of the interaction between increasing gestational age and obstetrical risk on birth outcomes: evidence of a varying optimal time of delivery. J Perinatol 26, 392–402 (2006). https://doi.org/10.1038/sj.jp.7211528
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jp.7211528
Keywords
This article is cited by
-
Geburtseinleitung
Monatsschrift Kinderheilkunde (2014)
-
Geburtseinleitung
Der Gynäkologe (2013)
-
Measuring perinatal complications: methodologic issues related to gestational age
BMC Pregnancy and Childbirth (2007)
-
What is the optimal gestational age for delivery?
Journal of Perinatology (2006)