Abstract
BACKGROUND: Since the introduction of the first protease inhibitor in January 1996, there has been a dramatic change in the treatment of persons infected with HIV. The changing nature of HIV care has important implications for the types of physicians that can best care for patients with HIV infection.
OBJECTIVE: To assess the association of specialty training and experience in the care of HIV disease with the adoption and use of highly active antiretroviral (ARV) therapy (HAART).
DESIGN: Observational cohort study of patients under care for HIV infection and their physicians.
PATIENTS AND SETTING: This analysis used data collected from a national probability sample of noninstitutionalized persons with HIV infection participating in the HIV Costs and Service Utilization Study and their primary physicians. We analyzed 1,820 patients being cared for by 374 physicians.
MEASUREMENTS: Rates of HAART use at 12 months and 18 months after the approval of the first protease inhibitor.
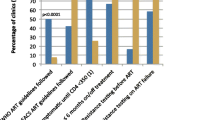
RESULTS: Forty percent of the physicians were formally trained in infectious diseases (ID), 38% were general medicine physicians with self-reported expertise in the care of HIV, and 22% were general medicine physicians without self-reported expertise in the care of HIV. The majority of physicians (69%) reported a current HIV caseload of 50 patients or more. In multivariable models controlling for patient characteristics, there were no differences between generalist experts and ID physicians in rates of HAART use in December 1996. When compared to ID physicians, however, patients being treated by non-expert general medicine physicians were less likely to be on HAART (odds ratio [OR], 0.32; 95% confidence interval [95% CI], 0.17 to 0.61). Patients being treated by low-volume physicians were also much less likely to be on HAART therapy than those treated by high-volume physicians (OR, 0.26; 95% CI, 0.14 to 0.48). These findings were attenuated by June 1997, suggesting that over time, the broader physician community successfully adopted HAART therapy. This finding is consistent with prior research on the diffusion of innovations.
CONCLUSIONS: Similar proportions of patients treated by expert generalists and ID specialists were on appropriate HAART therapy by December 1996 and July 1997. Patients treated by non-expert generalists, most of whom were the lowest-volume physicians, were much less likely to be on appropriate ARV therapy in the earlier time period. Our findings demonstrate that generalists who develop specialized expertise are able to provide care of quality comparable to that of specialists.
Similar content being viewed by others
References
Shapiro MF, Morton SC, McCaffrey DF, et al. Variations in the care of HIV-infected adults in the United States. Results from the HIV Cost and Services Utilization Study. JAMA. 1999;281:2305–15.
Carpenter CCJ, Fischl MA, Hammer SM, et al. Antiretroviral therapy for HIV infection in 1996. Recommendations of an international panel. International AIDS Society-USA. JAMA. 1996;276(2):146–54.
Carpenter CC, Cooper DA, Fischl MA, et al. Antiretroviral therapy in adults: updated recommendations of the International AIDS Society-USA Panel. JAMA. 2000;283:381–90.
Carpenter CC, Fischl MA, Hammer SM, et al. Antiretroviral therapy for HIV infection in 1997: updated recommendations of the International AIDS Society-USA panel. JAMA. 1997;277:1962–9.
Carpenter CC, Fischl MA, Hammer SM, et al. Antiretroviral therapy for HIV infection in 1998: updated recommendations of the International AIDS Society-USA Panel. JAMA. 1998;280:78–86.
Centers for Disease Control and Prevention. HIV AIDS Surveillance Report 11 (no. 1). Atlanta, Ga: U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention; 1999.
Palella FJ, Delandy KM, Moorman AC, et al. Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. N Engl J Med. 1998;338:853–60.
Bozzette SA, Joyce G, McCaffrey DF, et al. Expenditures for the care of HIV-infected patients in the era of highly active antiretroviral therapy. N Engl J Med. 2001;344:817–23.
Kitahata MM, Koepsell TD, Deyo RA, Maxwell CL, Dodge WT, Wagner EH. Physicians’ experience with the acquired immunodeficiency syndrome as a factor in patients’ survival. N Engl J Med. 1996;334:701–6.
Stone VE, Mansourati FF, Poses RM, Mayer KH. Relation of physician specialty and HIV/AIDS experience to choice of guideline-recommended antiretroviral therapy. J Gen Intern Med. 2001;16:360–8.
Kitahata MM, Van Rompaey SE, Shields AW. Physician experience in the care of HIV-infected persons is associated with earlier adoption of new antiretroviral therapy. J Acquir Immune Defic Syndr. 2000;24:106–14.
Bozzette SA, Berry SH, Duan N, et al. The care of HIV-infected adults in the United States. HIV Cost and Services Utilization Study Consortium. N Engl J Med. 1998;339:1897–904.
Frankel MR, Shapiro JF, Duan N, et al. National probability samples in studies of low-prevalence diseases. Part II: designing and implementing the HIV cost and services utilization study sample. Health Serv Res. 1999;34(5 Pt 1):969–92.
Shapiro MF, Berk ML, Berry SH, et al. National probability samples in studies of low-prevalence diseases. Part I: perspectives and lessons from the HIV cost and services utilization study. Health Serv Res. 1999;34:951–68.
Kish L. Survey Sampling. New York: John Wiley; 1965.
Lam NSN, Liu KB. Use of space-filling curves in generating a national rural sampling frame for HIV/AIDS research. Professional Geographer. 1996;48:321–32.
Duan N, McCaffrey D, Frankel M, et al. (RAND). HCSUS baseline methods technical report. In press.
Landon BE, Wilson IB, Wenger NS, et al. Specialty training and specialization among HIV physicians who treat HIV/AIDS in the United States. J Gen Intern Med. 2002;17:12–22.
American Medical Association. Available at: http://www.ama-assn.org/aps/amahg.htm. Accessed February 10, 2003.
Centers for Disease Control and Prevention. Guidelines for the Use of Antiretroviral Agents in HIV-Infected Adults and Adolescents. Department of Health and Human Services and Henry J. Kaiser Family Foundation. Morb Mortal Wkly Rep. 1998;47:43–82.
Report of the NIH panel to define principles of therapy of HIV infection. Ann Intern Med. 1998;128(12 Pt 2):1057–78.
Andersen R, Bozzette S, Shapiro M, et al. Access of vulnerable groups to antiretroviral therapy among persons in care for HIV disease in the United States. HCSUS Consortium. HIV Cost and Services Utilization Study. Health Serv Res. 2000;35:389–416.
Cunningham WE, Markson LE, Andersen RM, et al. Prevalence and predictors of highly active antiretroviral therapy use in patients with HIV infection in the United States. HCSUS Consortium. HIV Cost and Services Utilization Study. J Acquir Immune Defic Syndr. 2000;25:115–23.
Rubin DB. Estimating causal effects from large data sets using propensity scores. Ann Intern Med. 1997;127(8S):757–63.
Rogers EM. Diffusion of Innovations. 4th ed. New York: The Free Press; 1995.
Hnatiuk O, Moores L, Loughney T, Torrington K. Evaluation of internists’ spirometric interpretations. J Gen Intern Med. 1996;11:204–8.
Dolan NC, Martin GJ, Robinson JK, Rademaker AW. Skin cancer control practices among physicians in a university general medicine practice. J Gen Intern Med. 1995;10:515–9.
Ayanian JZ, Hauptman PJ, Guadagnoli E, Antman EM, Pashos CL, McNeil BJ. Knowledge and practices of generalist and specialist physicians regarding drug therapy for acute myocardial infarction. N Engl J Med. 1994;331:1136–42.
Chin MH, Friedmann PD, Cassel CK, Lang RM. Differences in generalist and specialist physicians’ knowledge and use of angiotensin-converting enzyme inhibitors for congestive heart failure. J Gen Intern Med. 1997;12:523–30.
Ayanian JZ, Guadagnoli E, McNeil BJ, Cleary PD. Treatment and outcomes of acute myocardial infarction among patients of cardiologists and generalist physicians. Arch Intern Med. 1997;157:2570–6.
Jollis JG, DeLong ER, Peterson ED, et al. Outcome of acute myocardial infarction according to the specialty of the admitting physician. N Engl J Med. 1996;335:1880–7.
Schreiber TL, Elkhatib A, Grines CL, O’Neill WW. Cardiologist versus internist management of patients with unstable angina: treatment patterns and outcomes. J Am Coll Cardiol. 1995;26:577–82.
Legorreta AP, Christian-Herman J, O’Connor RD, Hasan MM, Evans R, Leung KM. Compliance with national asthma management guidelines and specialty care: a health maintenance organization experience. Arch Intern Med. 1998;158:457–64.
Panush RS, Carias K, Kramer N, Rosenstein ED. Acute arthritis in the hospital: comparison of rheumatologic with nonrheumatologic care. J Clin Rheumatol. 1995;1:74–80.
Evans TI, Wheeler MT, Small RE, Breitbach SA, Sanders KM, Roberts WN. A comprehensive investigation of inpatient intravenous colchicine use shows more education is needed. J Rheumatol. 1996;23:143–8.
Vickrey BG, Edmonds ZV, Shatin D, et al. General neurologist and subspecialist care for multiple sclerosis: patients’ perceptions. Neurology. 1999;53:1190–7.
Norquist G, Wells KB, Rogers WH, Davis LM, Kahn K, Brook R. Quality of care for depressed elderly patients hospitalized in the specialty psychiatric units or general medical wards. Arch Gen Psychiatry. 1995;52:695–701.
Katz JN, Losina E, Barrett J, et al. Association between hospital and surgeon procedure volume and outcomes of total hip replacement in the United States Medicare population. J Bone Joint Surg Am. 2001;83:1622–9.
Jollis JG, Peterson ED, DeLong ER, et al. The relation between the volume of coronary angioplasty procedures at hospitals treating Medicare beneficiaries and short-term mortality. N Engl J Med. 1994;331:1625–9.
Hannan EL, Racz M, Ryan TJ, et al. Coronary angioplasty volume-outcome relationships for hospitals and cardiologists. JAMA. 1997;279:892–8.
Canto JG, Every NR, Magid DJ, et al. The volume of primary angioplasty procedures and survival after acute myocardial infarction. N Engl J Med. 2000;342:1573–80.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by grants from the Robert Wood Johnson Foundation, the Agency for Healthcare Research and Quality (grant no. R-01HS10227), and the Aetna Quality Forum, and by a cooperative agreement (U-01HS08578) between RAND and the Agency for Health Care Policy and Research. Dr. Bozzette is a Health Services Research and Development Senior Research Associate of the Department of Veterans Affairs.
Rights and permissions
About this article
Cite this article
Landon, B.E., Wilson, I.B., Cohn, S.E. et al. Physician specialization and antiretroviral therapy for HIV. J GEN INTERN MED 18, 233–241 (2003). https://doi.org/10.1046/j.1525-1497.2003.20705.x
Issue Date:
DOI: https://doi.org/10.1046/j.1525-1497.2003.20705.x