Index by author
PLAIN-LANGUAGE ARTICLE SUMMARIES
March-April 2023
Volume 21, Issue 1
Sarah M. Wood, and colleagues
Background Wood and Fiks, this issue’s editorialists, cite Aaron et al’s study about the greater effectiveness of vaginal, compared to urine, samples for molecular detection of sexually transmitted infections (STIs) in sex-at-birth females, and describe it as a necessary shift in practice.
What This Study Found They argue that transitioning to vaginal specimens in their patients could have a
critical health impact by increasing early treatment and reducing downstream transmission
of STIs. They assert that adopting more sensitive screening strategies also supports
two key tenets of reproductive justice for patients entering their peak reproductive
years, namely maintaining personal bodily autonomy and preserving the right to have
children when desired.
They note that chlamydia screening rates for U.S. adolescents are far below targets,
even using non-invasive urine testing. The authors call for the reduction of screening
barriers, such as limited visit time, confidentiality concerns, implicit bias and
clinician discomfort around discussing sexual health with adolescents. They also point
out that vaginal sampling may require teaching patients how to self-sample or for
clinicians to explain and collect specimens. Additionally, they foresee clinicians
having to manage parental expectations.
Implications
- Despite numerous barriers to vaginal testing implementation for STIs, Wood and Fiks affirm that Dr. Aaron et al provide sufficient data to demonstrate that defaulting to urine testing isn’t enough and that multiple cases of STI could go undetected. They recommend that vaginal testing be offered first and if it is not acceptable or feasible, then urine testing should be offered. “Family practitioners, pediatricians, and health systems will need to rise to this implementation challenge,” Wood and Fiks write. “By engaging now in implementation and quality improvement efforts with patients, physicians, clinic staff, and health systems, we can improve the quality, sensitivity, and reach of testing for adolescents and meaningfully improve adolescent health.”
Validity and Reliability of the Assessment of Burden of Chronic Conditions Scale in the Netherlands
Danny Claessens , and colleagues
Background Researchers evaluated the Assessment of Burden of Chronic Conditions (ABCC) scale, developed to improve care by facilitating shared decision making and self-management. The scale assesses and visualizes the patient’s experience of one or multiple chronic conditions, and integrates it in daily care. The researchers determined it is valid and reliable in people with Chronic Obstructive Pulmonary Disease (COPD), asthma or Type 2 Diabetes Mellitus (T2DM). They compared the ABCC scale with other clinical questionnaires to assess validity, consistency and reliability.
What This Study Found A total of 65, 62 and 60 people with COPD, asthma and T2DM, respectively, were included in the study. The ABCC scale correlated higher than the cut-off point for construct validity in 75% of the comparisons with the Saint George Respiratory Questionnaire; 100% of the comparisons with the Standardized Asthma Quality of Life Questionnaire (100%); and 75% of the comparisons with the Audit of Diabetes-Dependent Quality of Life Questionnaire. The team also found the ABCC scale was internally consistent and had good test-retest reliability for people with the three chronic conditions.
Implications
- The ABCC scale is a valid and reliable questionnaire that can be used within the ABCC tool for people with COPD, asthma or T2DM. They recommend that future research determine whether this applies to people with multimorbidity, and what the effects and experiences are upon clinical use.
Disparities in Shared Decision-Making Research and Practice: The Case for Black American Patients
Yaara Zisman-Ilani , and colleagues
Background To understand the perspectives of Black patients on shared decision making (SDM) during medical appointments, researchers and clinicians investigated the preferences, needs and challenges around SDM as experienced by Black individuals. The team also offers possible adaptations and modifications for SDM models, practice and research within Black communities. The study team recruited 32 Black patients – 18 men and 17 women – with type 2 diabetes from safety-net primary care clinics caring for medically underserved racial and ethnic communities. The team conducted qualitative interviews, asking about unmet needs, challenges and what might help in facilitating SDM. The team asked about issues related to race, culture and disparities. At the end of the interviews, participants completed the 9-item Shared Decision Making Questionnaire (SDM-Q-9).
What This Study Found Four themes emerged from the interviews: The first was preferences for humanistic communication. Participants reported a desire for their doctors to express empathy, concern and compassion as part of the medical appointment. They also wanted communications that utilized first names between doctors and patients and wanted “ice breaker” communications including humor and conversations with them rather than talking at them. The second theme that emerged was the need for doctors to account for the central role of family members in decision-making to facilitate adherence and engagement with the prescribed treatment. The third was the need for more medical information, specifically about tests and treatments; and the fourth theme was a growing mistrust in doctors, especially when patients felt unseen to the doctor or staff. Zisman-Ilani et al also suggested actions to help doctors better communicate with patients.
Implications
- The team argue that their findings offer meaningful and necessary insights and recommendations for future use and adaptations to make SDM more valuable in the care of Black patients and other ethnoracial minorities.
Proactive Recruitment Strategy for Patient Identification for Lung Cancer Screening
Traves Crabtree , and colleagues
Background Researchers examined the impact of a proactive patient education/recruitment program in a primary care setting on improving screening rates by low-dose computed tomography (LDCT) for lung cancer. They used a nurse navigator to help identify eligible patients for screening from the EMR and to contact them directly to provide preliminary pre-screening counseling and education on screening and smoking cessation.
What This Study Found Of the 451 current/former smokers in the study’s retrospective phase, 184 were eligible
for LDCT. Of the 184 patients, 34 had LDCT ordered; 32 completed LDCT; and 10 had
a lesion, while 150 did not undergo LDCT. In the prospective phase, among the 451
current/former smokers, 189 were eligible for screening; 22 had LDCT; 17 had a diagnostic
CT; and 150 required LDCT. The nurse navigator identified an additional 56 patients
as eligible upon contacting those with incomplete smoking histories. In total, 206
patients were eligible for LCDT, an increase of 37.3% compared to the retrospective
phase. Of the 206 eligible patients, 122 verbally agreed to screening; 94 met with
their physician; and 42 were prescribed a LDCT.
Researchers found that using a proactive education/recruitment model identified 37.3%
more eligible patients for LDCT. Fifty-nine percent of eligible patients verbally
agreed to a screening.
Implications
- The authors argue that it is essential to identify strategies, like the ones that they used, to increase LDCT screenings among willing and eligible patients.
Patient Satisfaction With Medical Care for Chronic Low Back Pain: A Pain Research Registry Study/b>
John C. Licciardone, and colleagues
Background Researchers measured the associations among process, outcomes and patient satisfaction within general medical care for chronic low back pain, provided through an ongoing patient-physician relationship. They also used two models to measure factors associated with patient satisfaction, including studying a subgroup of participants experiencing chronic low back pain who were being treated by the same physician for more than five years.
What This Study Found Among 1,352 participants, only physician empathy and physician communication were associated with patient satisfaction in the multivariable analysis that controlled for potential confounders. Similarly, in the subgroup of 355 participants, physician empathy and physician communication remained linked to patient satisfaction in the multivariable analysis.
Implications
- Physician empathy and physician communication were strongly associated with patient satisfaction with medical care for chronic low back pain. Researchers argue that patients with chronic pain highly value physicians who are empathic and who make efforts to more clearly communicate treatment plans and expectations.
Dee Mangin, and colleagues
Background Researchers evaluated the feasibility of implementing the Health TAPESTRY (Health
Teams Advancing Patient Experience: STRengthening QualitY) primary care program across
multiple sites, and the reproducibility of the effects found in a previous randomized
controlled trial (RCT). Health TAPESTRY is aimed at helping older adults stay healthier
longer. The study was a pragmatic, unblinded, six-month parallel group RCT. Eligible
patients were 70 years and older, receiving care from one of six participating interprofessional
primary care practices (both urban and rural). In total, 599 patients (301 intervention,
298 control) were recruited from March 2018-August 2019. Intervention participants
received a home visit from volunteers to
collect information on physical and mental health, as well as their social environment.
An interprofessional care team then created and implemented a care plan. The primary
outcomes were the amount of physical activity and number of hospitalizations.
What This Study Found Researchers found that Health TAPESTRY had widespread reach and adoption, based on
the RE-AIM (Reach, Effectiveness, Adoption, Implementation, and Maintenance) framework.
In the intention-to-treat analysis (257 intervention, 255 control), there were no
statistically significant between-group differences for hospitalizations and total
physical activity. There were 37 non-study related serious, adverse events (19 intervention,
18 control).
Implications
- The authors found Health TAPESTRY was successfully implemented in diverse primary care practices. However, implementation did not reproduce the effect on hospitalizations and physical activity found in the initial randomized control trial.
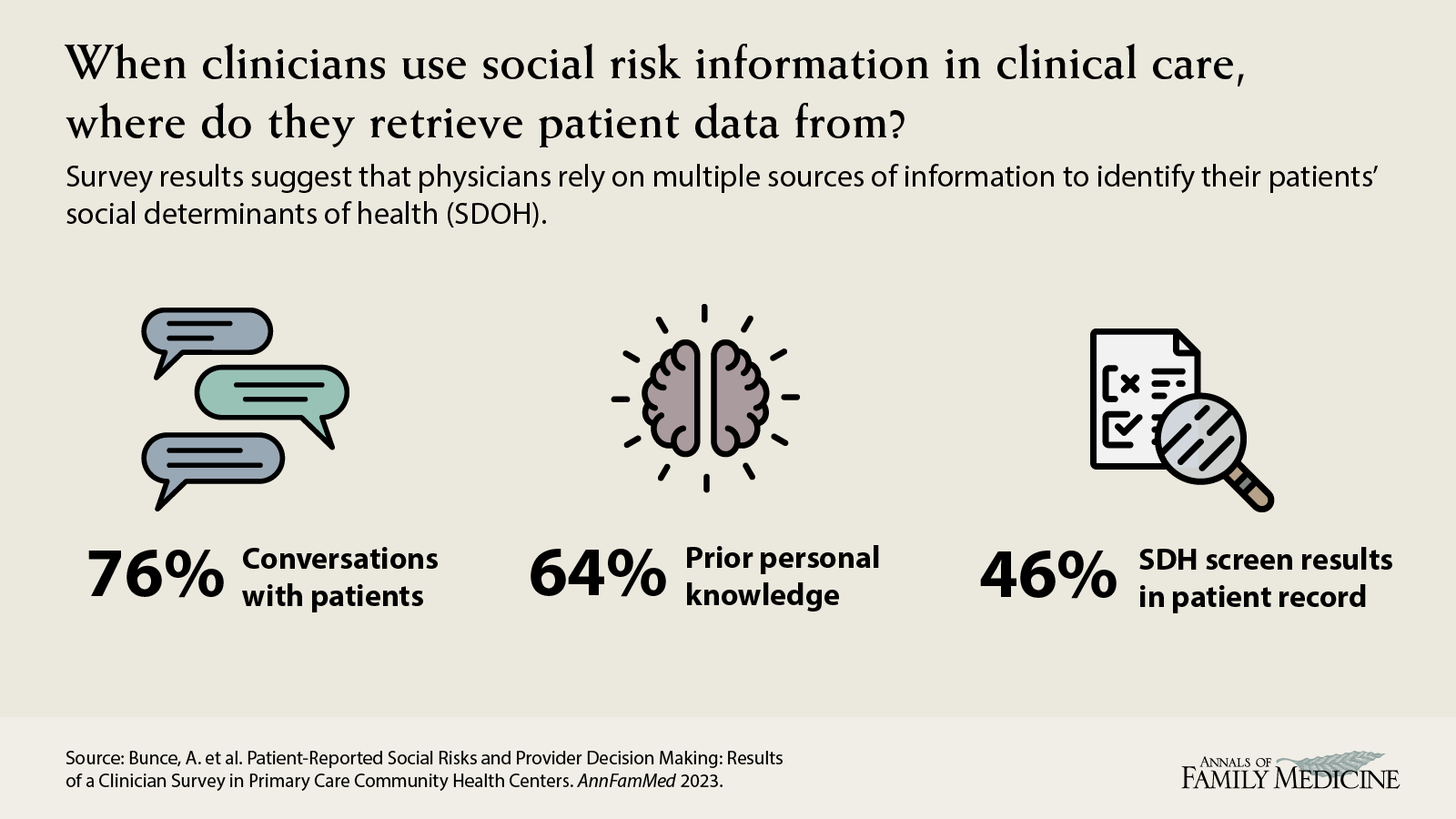
Arwen Bunce , and colleagues
Background A recent study conducted in a large nonprofit network of community health centers assessed the extent to which patients’ social determinants of health influence safety-net primary care clinicians’ decisions at the point of care, and how that information came to the clinician's attention. Descriptive statistics and generalized estimating equation models were used to assess relationships between clinician, patient and encounter characteristics and clinicians’ reported use of social determinants of health data in clinical decision-making.
What This Study Found Social determinants of health influenced care in 35% of surveyed encounters. Most common sources of information on patients’ social determinants of health were conversations with patients (76%); prior knowledge of the patient’s social determinants of health (64%); and social determinants of health information documented in the EHR (46%). Social determinants of health were significantly more likely to influence care for male and non-English-speaking patients, and those with social determinants of health screening data documented in discrete (i.e., more easily measurable and reportable) fields in the EHR.
Implications
- EHRs present an opportunity to support clinicians in integrating information about patients’ social and economic circumstances into care planning.
M. Ruth Lavergne, and colleagues
Background Canadian researchers describe changes in the comprehensiveness of services delivered by family physicians in four Canadian provinces (British Columbia, Manitoba, Ontario, and Nova Scotia) between 1999/2000 and 2017/2018, and explore if changes differ by the number of years physicians are in practice. They argue that having an accurate picture of changes in comprehensiveness can inform policy responses. They measured comprehensiveness using province-wide billing data across seven settings (home, long-term care, emergency department, hospital, obstetrics, surgical assistance, anaesthesiology) and seven service areas (pre/post-natal care, pap testing, mental health, substance use, cancer care, minor surgery, and palliative home visits).
What This Study Found They found that comprehensiveness declined in all provinces, with greater changes
in the number of settings than service areas. Declines were no greater among new-to-practice
physicians than those who had 10 or more years of service. While comprehensiveness
has declined over time among physicians entering practice, this decline occurred across
all career stages in the study’s time periods. Findings are consistent across the
four Canadian provinces the team examined.
Implications
- The authors argue that any efforts to enhance or maintain comprehensive family medicine services should address the service delivery contexts in which all primary care physicians are practicing, rather than interventions in training or early practice.
Characteristics of Family Physicians Practicing Collaboratively With Behavioral Health Professionals
Sebastian T. Tong, and colleagues
Background Researchers from the American Board of Family Medicine (ABFM) and the University of Washington in Seattle examined the characteristics of family physicians who work collaboratively with behavioral health professionals (BHP). Prior evidence has demonstrated that integrating behavioral health into primary care can improve access to mental health care and patient health outcomes.
What This Study Found Almost 40% (38.8%) of 25,222 family practitioners reported working collaboratively with behavioral health professionals. Physician characteristics significantly associated with increased odds of BHP collaboration were being female (OR 1.09) and working as core/salaried faculty (OR 2.32) as compared to non-faculty. The strongest practice characteristic was working in a federally run practice site and the strongest negative association was working in an independently owned practice and being located in the Southern United States. Additionally, working in a county with more psychiatrists is associated with higher likelihood of BHP collaboration.
Implications
- Understanding these disparities could help improve behavioral health access for patients and improve overall patient outcomes.
Impact of COVID-19 Pandemic on Assessing Tobacco Status in Community Health Centers/b>
Susan A. Flocke, and colleagues
Background Researchers from Oregon Health & Science University and OCHIN, a large nonprofit network of community health centers, extracted electronic health record data from 217 primary care clinics between January 2019 through the end of July 2021, which included telehealth and in-person visits for 759,138 adult patients aged 18 and older years to determine how monthly rates of tobacco assessment had been affected by the COVID-19 pandemic. The team calculated the rates per 1,000 patients.
What This Study Found The team found that between March and May 2020, tobacco assessment monthly rates declined from 155.7 per 1,000 patients down to 77.7 per 1,000 patients, a 50% decline. There was a subsequent increase in tobacco assessment between June 2020 and May 2021. However, assessments remained 33.5% lower than pre-pandemic levels.
Implications
- The decline in the rate of tobacco assessments during the onset of the COVID-19 pandemic
was substantial and rates have yet to return to pre-pandemic levels. Given that tobacco
use can exacerbate COVID-19 symptoms, researchers recommend careful examination of
procedural changes to adapt care delivery to support community health centers, specifically
tobacco cessation efforts.
Michael J. Barry , and colleagues
Background A team of current and former U.S. Preventive Services Task Force (USPSTF) members and staff from the Agency for Healthcare Research and Quality describe how USPSTF methods are evolving to address preventive health equity and define evidence gaps for future research. The USPSTF uses rigorous methods including comprehensive, systematic reviews addressing the benefits and harms of specific preventive services. The task force’s recommendations are used by primary care clinicians and their patients to decide together which preventive strategies are right for each person.
What This Study Found The team discusses how the USPSTF prioritizes topics based on disease burden; extent of new evidence; whether the service can be provided in primary care; and how, going forward, members will increasingly consider health equity. The task force uses analytic frameworks to specify key questions and linkages connecting a specific preventive service with health outcomes. Contextual questions help provide information on natural history, current practice, health outcomes in high-risk groups, and health equity. The task force assigns a level of certainty to the estimate of net benefit of a preventive service: high, moderate, or low. The magnitude of net benefit is also judged based on whether those benefits minus harms are substantial, moderate, small or zero/negative. The USPSTF uses these assessments to assign a letter grade from ‘A’ (recommend) to ‘D’ (recommend against). ‘I’ statements are issued when evidence is insufficient to recommend for or against a service.
Implications
- The authors report that the USPSTF will continue to evolve its methods for simulation modeling and the use of evidence to address conditions where there is limited data for specific groups that bear a disproportionate burden of disease. Additional pilot work is underway to better understand the relationship of the social constructs of race, ethnicity and gender to health outcomes to further inform the development of a USPSTF health equity framework.
Kristal J. Aaron , and colleagues
Background Researchers conducted a meta-analysis of multiple databases from 1995-2021 to assess
the diagnostic sensitivity of commercially available tests that use vaginal swabs
versus urine specimens to detect chlamydia, gonorrhea and trichomonas. Although vaginal
swabs are the recommended sample type by the Centers for Disease Control and Prevention
(CDC),, the most used specimen among women is urine. The authors identified 28 eligible
articles with 30 comparisons for CT; 16 comparisons for NG; and nine comparisons for
TV.
What This Study Found Vaginal swabs consistently performed somewhat better than urine tests in detecting STIs; however, for trichomonas, the odds ratio that vaginal swabs were more sensitive than urine did not reach statistical significance. For vaginal swabs and urine, respectively, pooled sensitivity estimates were 94.1% and 86.9% for CT; 96.5% and 90.7% for NG; and 98.0% and 95.1% for TV. The differences were statistically significant for chlamydia and gonorrhea.
Implications
- The authors assert that this analysis supports the CDC’s recommendation that vaginal
swabs are the optimal sample type for women being tested for chlamydia, gonorrhea
and/or trichomonas. Relying on urine testing could result in an estimated 400,000
undetected cases of chlamydia and gonorrhea each year. While vaginal swab tests are
the most sensitive for STI testing, urine testing is a reasonable alternative when
swabs are not available or acceptable.
Forging a Social Movement to Dismantle Entrenched Power and Liberate Primary Care as a Common Good
Kevin Grumbach
Background In this essay, Kevin Grumbach, MD, argues that it is unreasonable for family physicians and their allies committed to ensuring that all Americans have access to high-quality primary care to overcome decades of policy failures without adopting different tactics to change those policies. He contends that primary care is a common good, echoing the position of the National Academies of Sciences, Engineering, and Medicine report on primary care published in 2021. However, he asserts that a profit-oriented, market-based health system does not promote primary care as a common good and in fact serves as a structural barrier to reaping primary care’s benefits.
What This Study Found He issues a bold call for a Primary Care for All program – a tax-financed system of
universal coverage for primary care funded at twice the level of current spending
on primary care in the US. He adds that professionalism in primary care has both aided
and constrained those in the profession and that primary care doctors must embrace
what he calls “counterculture professionalism” to join with fellow primary care workers,
patients and other partners to build a broad social movement to challenge entrenched
interests and demand fundamental restructuring of the health system and the democratization
of health.
“Family physicians must ignite a flame of ‘counterculture professionalism’ to exercise
moral authority and be trustworthy partners in a democratic movement to liberate primary
care as a common good,” Grumbach writes. “The path to well-supported primary care
will not be found in taking comfortable roads that, in the past, never arrived at
their desired destination.”
Integrating Behavioral Health and Primary Care: Turning a Duet Into a Trio
Anne C. Jones , and colleagues
Background Family physician Anne C. Jones, DO, and behavioral health consultant Kaitlin Lilienthal, PhD, describe a practice transformation that improved care experiences. Working closely together in a Primary Care Behavioral Health Model within a university setting, the authors describe their collaborative approach to helping a college student with a complex mix of physical and psychological symptoms. Similar to a musical ensemble, the authors describe key details of interdisciplinary collaboration that promotes holistic care for patients and a fulfilling biopsychosocial practice.
What This Study Found Many patients present with both physical and psychological symptoms in family practice settings. Integrated behavioral health can address all of the patients’ concerns in a coordinated way.
Implications
- When health care teams work together to implement behavioral health into primary care (such as having a behavioral health consultant work with a primary care doctor in the same office), they can knit together a fragmented health care system and help patients overcome barriers to care.
Implementing Whole Person Primary Care
Elena Rosenbaum , and colleagues
Background The HOPE Note Toolkit is being used in some healthcare systems to improve whole person care.
What This Study Found In order to support clinics in the process of adopting the HOPE Note Toolkit in primary care, researchers tested a learning collaborative approach across 17 primary care clinics in the United States, including private practices and family medicine residency training programs. The collaborative used expert and peer supported practice improvement and action research to help clinical teams develop the skills and processes needed to conduct whole person integrative health visits using the toolkit. The 16 participating clinics represented more than 220 clinicians serving approximately 39,000 patients.
Implications
- Most clinics planned to expand their use of the tools and reported improved knowledge, skills and delivery of whole person care.

